UVM News brings you the University of Vermont’s top stories, showcasing breakthrough research, timely solutions and experts, and news from Vermont’s flagship university.
Featured News

Naturally Fearless? A UVM Neuroscientist on How Elite Athletes View Risk
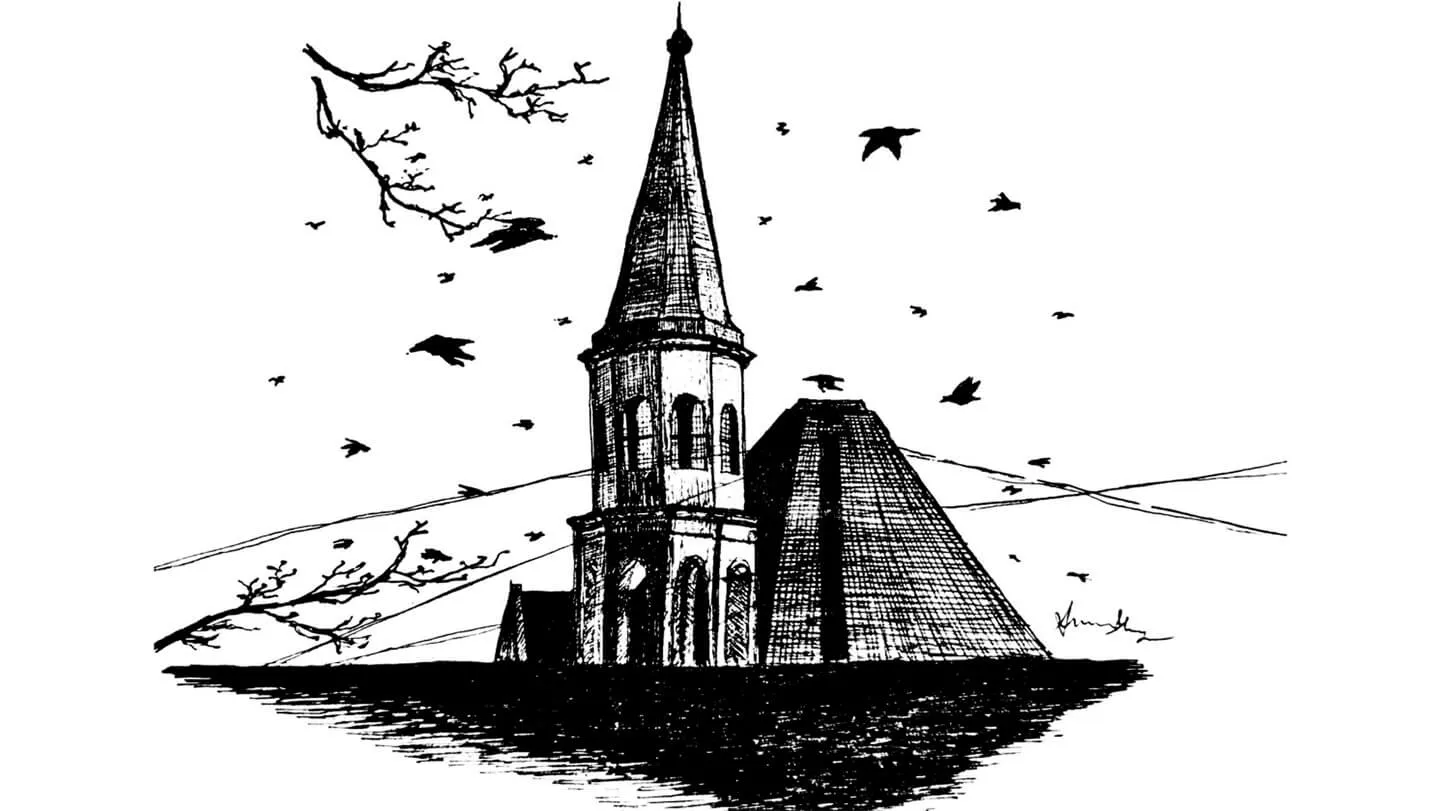
Caw of the Wild: Students Study Crows Around Burlington

Toward a Bold Future: UVM Charts its Path with “Green, Gold, and Bold” Strategic Plan

Three UVM Athletes Medal at the 2026 Winter Olympics, Ogden Brings Home Second Silver

Catamount LEAP Project Update: Building on Input from Throughout the Campus Community















