UVM News brings you the University of Vermont’s top stories, showcasing breakthrough research, timely solutions and experts, and news from Vermont’s flagship university.
Featured News

Catamounts Notch Record Performance in 2026 Winter Olympics

Naturally Fearless? A UVM Neuroscientist on How Elite Athletes View Risk
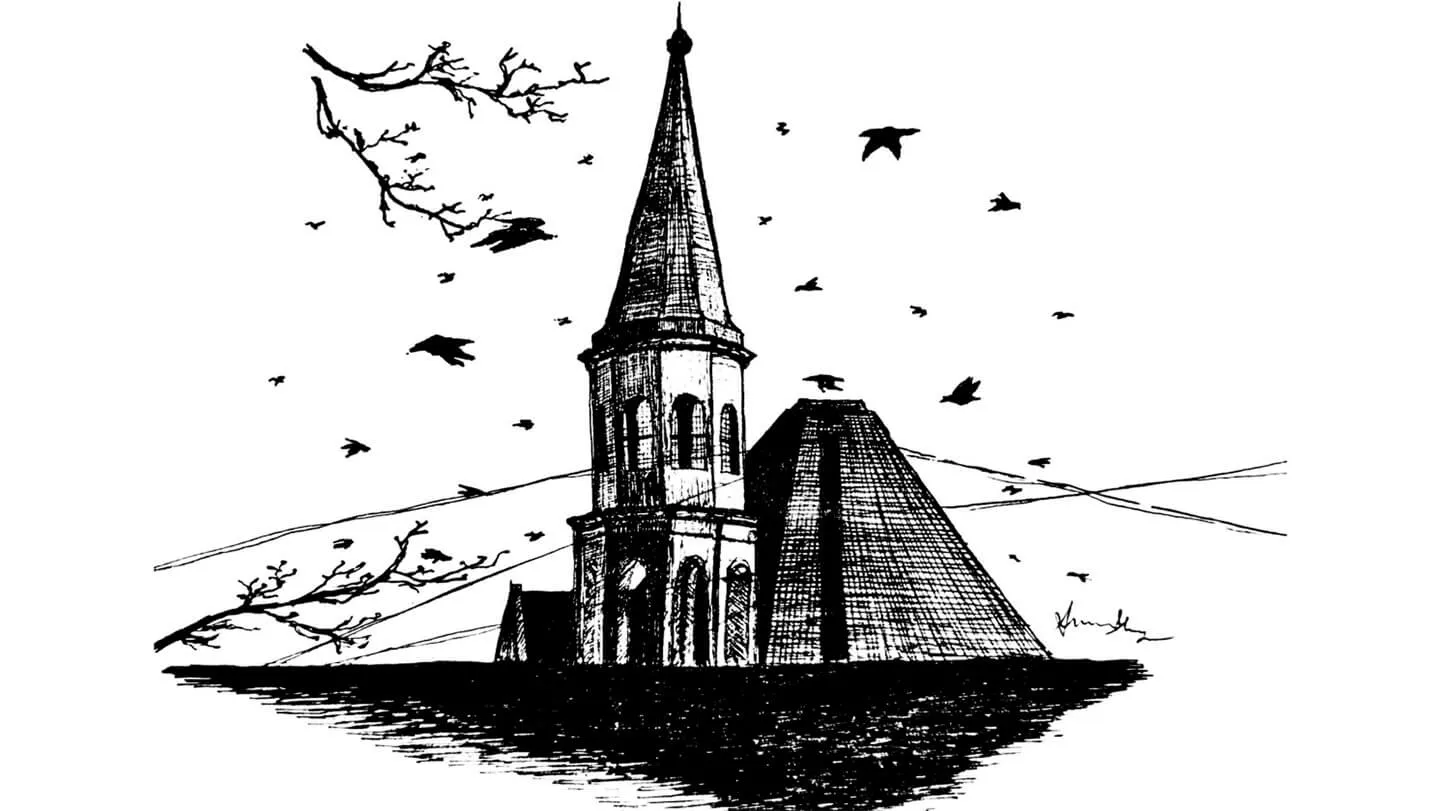
Caw of the Wild: Students Study Crows Around Burlington

Toward a Bold Future: UVM Charts its Path with “Green, Gold, and Bold” Strategic Plan

Three UVM Athletes Medal at the 2026 Winter Olympics, Ogden Brings Home Second Silver















