Extensive research focuses on the role of and mechanisms underlying thrombosis and inflammation in ischemic heart disease. Platelets are pivotal in thrombosis, and antiplatelet agents are pivotal in the treatment of ischemic heart disease. Paradoxically, however, our ability to assess platelet function and to quantify effects of antiplatelet agents is limited.
Our group has developed a sensitive and specific method to assess platelet function. With the assay developed, we have demonstrated that assessment of the potential for platelets to activate (i.e. platelet reactivity) can be used to identify patients at high and low risk of subsequent cardiac events. We have used this approach to define more effective modes of treatment for patients with acute coronary syndromes.
Our group is actively involved in defining optimal anti-thrombotic therapy with both anticoagulants, and antiplatelet agents. Research efforts range from mechanistic studies in vitro to translational studies designed to apply novel laboratory methods to improve treatment and clinical trials testing the efficacy of novel therapeutic agents and combinations.
We have developed and validated methods by which biochemical quantification of the extent of myocardial infarction can be accomplished in vivo based on sequential analyses of concentration in plasma of macromolecules (CK, MB CK isoenzymes, and other moieties such as troponin I and troponin T) and applied them to determine the extent of infarction is an important determinant of prognosis after myocardial infarction and furthermore, whether the extent of infarction can be modified by interventions that reduce myocardial oxygen requirements or increase myocardial oxygen supply.
This work has had a major impact on how patients with acute myocardial infarction are treated and led to a reduction of mortality secondary to treatments, such as thrombolysis that were validated initially with the methods developed.
We have contributed to the initial development of cardiac positron emission tomography with the use of positron-emitting radionuclides including carbon-11 labeled palmitate, the physiological fuel of myocardium, and applied it to further delineate the nature of evolution of infarction and its interdiction with interventions salvaging ischemic myocardium including coronary thrombolysis with clot-selective fibrinolytic agents.
We have pioneered coronary thrombolysis with the use of the clot-selective plasminogen activator, tissue-type plasminogen activator (t-PA), in studies of cells in culture, experimental animals, and mechanistic clinical studies in patients with acute myocardial infarction with quantification of the extent of infarction by positron emission tomography and analysis of time activity-curves in blood of enzymes liberated from myocardium. This work provided a foundation for subsequent large-scale, multicenter clinical trials in which Dr. Burton Sobel helped to demonstrate the efficacy of coronary thrombolysis with clot-selective agents, heparin, and aspirin in the reduction of death associated with coronary artery disease and acute myocardial infarction.
Recently we delineated altered fibrinolysis in blood and altered proteolytic activity in vessel walls as mediators of deleterious effects of hyperinsulinemia associated with insulin resistance, impaired glucose tolerance, and type 2 diabetes, thereby helping to elucidate the pathophysiology of macrovascular angiopathy in type 2 diabetes. This work, coupled with results of studies demonstrating that insulin sensitizers normalize fibrinolysis in patients with type 2 diabetes, is changing the approach to their treatment directed at reducing the risk of heart attack and cardiac death.
Platelet Biology, Coagulation, and Fibrinolysis
We have demonstrated that the combination of hyperinsulinemia, hyperglycemia and increased concentrations of free fatty acids in blood of healthy subjects increases the concentration and activity of the primary inhibitor of fibrinolysis, plasminogen activator inhibitor type-1.
In vitro studies delineated that increased concentrations in blood of insulin increase expression of PAI-1 through stabilization of mRNA. In addition, we demonstrated that free fatty acids increase expression of PAI-1 by increasing transcription of PAI-1 through a fatty acid response region in the 5’ untranslated region of the PAI-1 gene.
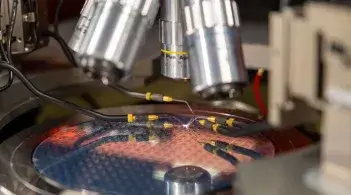
In addition, we have developed a semi-quantitative method to assess plaque morphology in mice. This approach has been implemented to determine the role of genetic modifications such as increased vascular smooth muscle expression of PAI-1 in the genesis of atherosclerotic lesions. We have developed and implemented a sensitive and specific means for assessment of platelet function that utilizes flow cytometry to characterize specific components of platelet reactivity. Our work has utilized this method to delineate the prognostic implications of platelet reactivity and to characterize the effects of selected treatment modalities on platelet function and prognosis.