Despite years of research to improve treatment, the prognosis for patients with lung cancer remains poor, in part due to the reality that lung cancer is not a single disease. In fact, at the genomic level, each patient’s lung cancer is unique.
Genomic tumor sampling offers helpful prognostic information for clinicians and aids in tailoring treatment plans. But the sheer volume of data accumulated presents interpretive challenges, particularly in cases where a documented genetic alteration’s clinical significance is unclear. The ability to characterize these “variants of uncertain significance,” or VUS, is an important step in enhancing patient care through precision medicine, and the focus of a collaborative study between the labs of UVM researchers Paula Deming, Ph.D., MT (ASCP), and David J. Seward, M.D., Ph.D.
Seward’s work in clinical medical interpretation of tumor genotypes and Deming’s background in molecular signaling networks provided a natural synergy for the research. Together, the team has established new genomic biomarkers that predict certain lung cancers’ sensitivity to available therapies, clarifying effective courses for treatment.
Published in the journal Carcinogenesis: Integrative Cancer Research, Deming and Seward’s study focuses on STK11, a protein that regulates normal homeostasis in lung tissue - and what happens when the gene that encodes for the protein is genetically altered. Using data obtained from next generation sequencing of human lung tumor biopsies from University of Vermont Medical Center patients, the researchers identified 32 VUS in the STK11 gene.
“A mutation, or genetic alteration, in the DNA can cause a change in the function of the protein such that the protein can't work anymore,” Deming explains. When the function of the protein is to suppress tumor development, the altering mutation may lead to the opposite – tumor progression.
Genetic alterations in certain genes like STK11 are associated with lung cancer progression, says Deming. The importance of documenting the effects of these understudied VUS in tumor suppression guided the team’s work in sequencing the biopsy data.
“STK 11 was one of the gene sequences studied because we know that when the function of this gene product or the protein is lost, people present with a more aggressive lung cancer, and there's also evidence to suggest they don't respond to the leading therapy, which is immunotherapy,” said Deming.
“In the case of STK11, clinically relevant alterations in the gene render it non-functional,” said Seward. “As a result, there is need to establish rapid protocols to determine whether a previously uncharacterized variant alters function.”
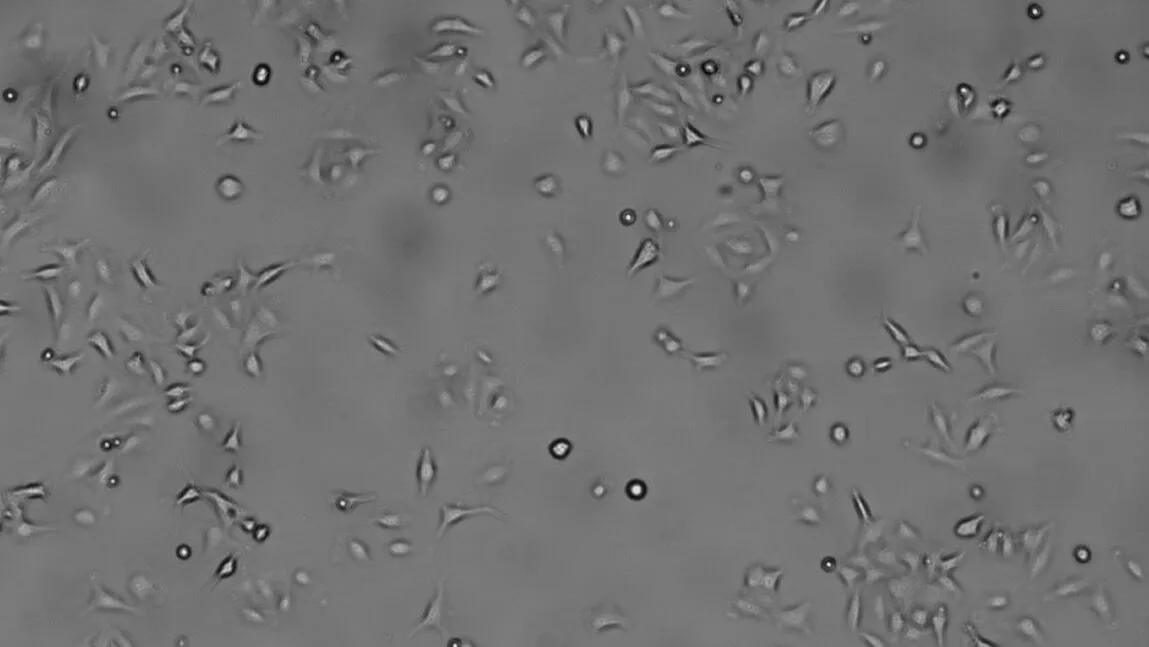
By cloning and expressing the STK11 VUS in lung cancer cell lines that lack the STK11 protein, the researchers can measure the impact of these genetic variations on STK11 enzyme activity and signaling that prevents the activation of tumor pathways.
“We can categorize these genetic variants as being pathogenic or benign,” said Deming. “That's very useful for the clinicians because it helps provide information on prognosis and can help guide treatment plans.”
And while the technology to conduct sequencing rapidly, accurately, and affordably is available, Seward explains the task of accurate interpretation remains a challenge to be overcome.
“We currently struggle to accurately assess variants in single genes. Attempting to integrate multiple variants in all genes across the genome is a dream,” Seward said. “But a dream we may see come true.”
Work following this publication will focus on understanding the downstream molecular effects imparted by STK11 functional disruption, says Seward: “We hope that by revealing and understanding these pathways we can reinstate the effectiveness of anti-PD-1 antibody therapy in KRAS-driven lung adenocarcinomas lacking functional STK11.”
The team’s findings will be added to a national database of identified tumor sequences and recommended therapies used by clinicians in determining courses of treatment.
Paula Deming, Ph.D., MT (ASCP), is Associate Professor and Endowed Professor of Health Sciences in the Department of Biomedical and Health Sciences, and Associate Dean for Faculty Affairs and Research in the College of Nursing and Health Sciences.
David Seward, M.D., Ph.D., is the Elmer R. Huber Early Career Green and Gold Professor in Pathology and Laboratory Medicine and Assistant Professor in the University of Vermont Department of Pathology and Laboratory Medicine.