Larner Researchers Share Key Discoveries on Impacts of Lifestyle and Epidemiology on Cardiovascular Health
Medical students, postdoctoral fellows and associates, and faculty from the UVM Larner College of Medicine presented a record 14 research projects at the American Heart Association Epidemiology and Prevention | Lifestyle and Cardiometabolic Health scientific sessions in New Orleans March 6–8, 2025. The event provided a venue for cardiovascular health researchers to share their key discoveries and network with expert peers.
Presentations by Medical Students
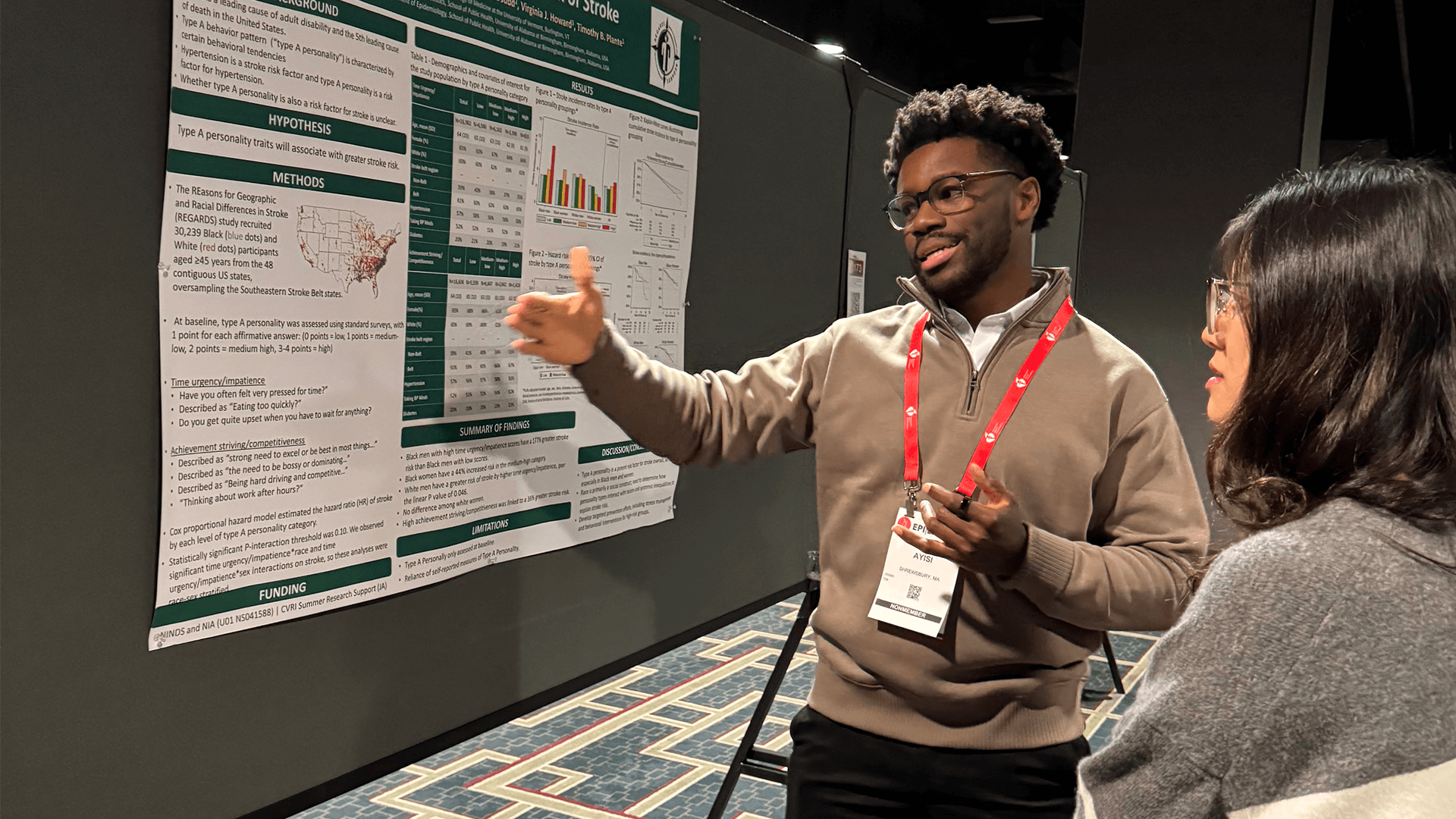
Jake Ayisi ’27
Type A Behavior Pattern and Incident Stroke: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study
Type A personality has been linked to hypertension, which is a known risk factor for stroke. New research led by Ayisi assessed aspects of Type A personality and risk of stroke in American adults. Associations were most prominent in Black men. For example, those who were more impatient had nearly twice the risk of stroke. Those with greater drive to work hard and succeed had a slightly increased risk. More research is needed to understand the causes and reasons for observed race/sex differences. Tim Plante, M.D., M.H.S., served as faculty mentor for Ayishi, whose research was supported by a Cardiovascular Research Institute fellowship.
Vinh Le ’24
Atrial Fibrillation and Risk of Incident Cognitive Impairment: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study
Atrial fibrillation (AFIB) affects millions of older adults in the U.S. This study showed that in people with a prior stroke, AFIB was associated with increased risk of developing future cognitive impairment. This was not the case in the absence of prior stroke. Future research should aim to determine if interventions to preserve cognitive function in those with AFIB and stroke will be effective.
Biomarkers and Risk of Cognitive Impairment in Atrial Fibrillation: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort
In a separate investigation of more than 2000 people with AFIB, Le found that increased levels of three blood biomarkers were each associated with risk of developing cognitive impairment in people with AFIB. One of the biomarkers, called GDF-15, is a marker of inflammation, and investigators found that anticoagulation treatment might protect against cognitive problems in people with higher GDF15. Results show factors that link heart and brain health. Mary Cushman, M.D., M.Sc., served as Le’s faculty mentor for both projects, which received support from philanthropic funds.
Erin Manogaran ’27
A Measure of Residential Segregation and Thrombo-inflammation in Black and White Americans
Black women in the U.S. face the highest rates of hypertension, with racial disparities in inflammatory responses contributing to risk. Manogaran’s study showed that a measure of residential segregation was associated with lower levels of IL-1β, a key thrombo-inflammatory biomarker related to hypertension. These findings suggest that living in majority Black counties may offer protective effects for Black people. Manogaran’s research was supported by a Cardiovascular Research Institute fellowship, and Debora Kamin Mukaz, Ph.D., served as faculty mentor.
Elizabeth Pendlebury ’27
Racial Differences in the Impact of Elevated Systolic Blood Pressure on Incident Cognitive Impairment (ICI) Risk: The REGARDS Study
Black Americans have the highest rate of hypertension of any racial/ethnic group in the world. Hypertension is a risk factor for cognitive impairment. Pendlebury hypothesized that elevated systolic blood pressure is a stronger risk factor for incident cognitive impairment in Black than White adults. They found that elevated systolic blood pressure was associated with increased risk for developing cognitive impairment, but the risk was equal for Black and White adults. These findings contrast with other research showing a stronger association of blood pressure with stroke in Black than white people. Nels Olson, Ph.D., served as faculty mentor for Pendlebury, whose research was supported by a Cardiovascular Research Institute fellowship.
Rhea Puthumana ’27
Pro-Enkephalin A and Risk of Incident Hypertension: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study
Hypertension is a major risk factor for cardiovascular disease and chronic kidney disease and is a significant burden globally. Puthumana investigated if the biomarker pro-enkephalin A predicted an increased risk of hypertension because it is involved in kidney dysfunction. Findings showed that pro-enkephalin A did not substantially increase risk for hypertension. Puthumana and faculty mentor Tim Plante, M.D., M.H.S., suggest that future research should aim to understand associations of pro-enkephalin A with cardiovascular disease risk, especially in those with kidney disease. Puthumana’s project was supported by a Cardiovascular Research Institute fellowship.
Eric Stoutenberg ’25
Factor IX and Incident Hypertension in Black and White Adults: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort
In research led by Stoutenberg, a higher blood level of a pro-clotting factor called factor IX was associated with an increased risk of future hypertension. This demonstrates possible new roles for factor IX that might aid in reducing the burden of hypertension in the future. Tim Plante, M.D., M.H.S., served as faculty mentor on this research.
Evelyn Thomas ’27
Impact of the Delta Index, a Measure of Residential Segregation, on Hypertension Risk Among Black and White Women and Men
High blood pressure is a major public health concern, with persistent disparities affecting Black Americans and women in the U.S. Thomas, with the mentorship of Debora Kamin Mukaz, Ph.D., investigated whether living in segregated neighborhoods affects the risk of developing high blood pressure differently for Black and white women and men. Counter to their hypothesis, they found that Black women living in more segregated areas had a lower risk of developing high blood pressure. Future research will help increase understanding of this unexpected relationship. This project was supported by a Cardiovascular Research Institute fellowship.

Presentations by Faculty and Postdoctoral Fellows and Associates
Andres Cordova Sanchez, M.D., Clinical Instructor of Medicine, Cardiology Fellow
Blood Biomarkers and the Risk of Coronary Disease in Atrial Fibrillation
Cordova Sanchez, a cardiovascular disease fellow mentored by Mary Cushman, M.D., M.Sc., investigated the risk of heart attack in AFIB. They found that, in more than 2000 people with AFIB, multiple laboratory biomarkers predicted the risk of heart attack. Next steps will involve seeing if any of these might be useful in clinical practice to reduce heart attack risk in AFIB.
Mary Cushman, M.D., M.Sc., University Distinguished Professor of Medicine and Pathology & Laboratory Medicine
Pre-Pandemic Thrombo-inflammatory Biomarkers and Risk of Severe Covid-19: The Collaborative Cohort of Cohorts for COVID-19 Research
In people hospitalized with COVID-19, those with more inflammation have a higher mortality rate. Cushman led a study of 12 long-term cohorts that shows inflammation levels measured 20 years before the pandemic predicted the chance that a person would develop severe COVID-19 requiring hospitalization. These findings provide new insights into susceptibility to severe illness from a virus.
Minaz Mawani, Ph.D., M.P.H., B.Sc.N., Postdoctoral Associate, Department of Medicine
Determining Decision Thresholds of Physicians and Parents for Instituting a Do-Not-Attempt-Resuscitation Order for Pediatric In-Hospital Cardiac Arrest Patients: A Cross-Sectional Study of Parents and Physicians in the United States
Decision-making about resuscitating a hospitalized child is difficult and complex. Mawani conducted a survey of physicians and parents across the United States and found that physicians tend to overestimate how likely it is that a critically ill child will survive. The survey also found that parents would want their child resuscitated even in situations where the chance of survival is so low that the physician would not recommend trying to resuscitate.
Out-ofHospital Pediatric Cardiac Arrest, Survival, and Associated Factors: A Systematic Review and Meta-Analysis
Out-of-hospital cardiac arrest in children has poor survival and neurological outcomes. Mawani evaluated 20 years of published data and found that only one in eight of these children survived, and 16 of 17 had poor neurological outcome. Survival was higher among children in Europe than in North America, Asia, and Australia. Quality of the literature could be improved with use of uniform reporting criteria.
Tim Plante, M.D., Assistant Professor of Medicine
Empirically Derived Biomarker Patterns in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study and Incident Hypertension by Biomarker Patterns: Reasons for Geographic and Racial Differences in Stroke REGARDS Study
While risk factors for hypertension are well described, its cause remains elusive. Plante’s research team identified three naturally occurring patterns of blood biomarkers representing abnormal biology of different organ systems related to onset of hypertension. Specifically, these three patterns all related to inflammation and involve blood clotting, kidney disease, and high cholesterol. These patterns were identified in 1223 Black and White adults free from hypertension. Persons with strong signals for the blood clotting–inflammation pattern and the cholesterol–inflammation pattern had the greatest risk of developing hypertension. The authors concluded that the origins of hypertension might relate to adverse inflammation that co-exists with adverse blood clotting and high cholesterol.
