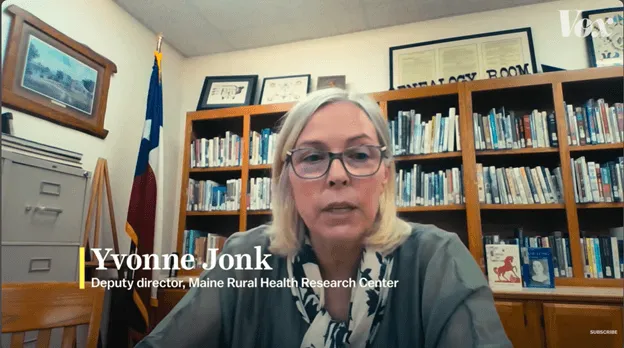
Yvonne Jonk, PhD, co-director of the Northeast Rural Health Research Center (NeRHRC), recently spoke with Vox about her research on “ambulance deserts”, regions in the U.S. where it takes more than 25 minutes for emergency medical services (EMS) to reach a patient. An estimated 4.5 million people live in these underserved areas.
While geography plays a role, much of the problem stems from systemic design flaws. Unlike police and fire departments, which are considered “essential services” and funded by tax dollars, EMS is not classified the same way. As a result, EMS providers rely on reimbursement from insurance companies or direct payments from patients.
"There are areas of the state where you do not want to, you know, have an accident, because there's no one - no one will be coming. At least, not in a timely manner." - Yvonne Jonk, PhD
Compounding the issue, EMS agencies are typically only reimbursed if they transport a patient to a hospital. If a patient declines transport, the provider often receives no compensation despite incurring the same costs. This model disproportionately affects rural EMS providers, who face lower call volumes and limited funding, yet must maintain the same readiness and infrastructure as their urban counterparts.
In many rural communities, EMS services are staffed by volunteers due to insufficient funding for full-time positions. It is suggested that a key step toward solving this crisis may be reclassifying EMS as an essential service. Doing so could unlock public funding and ensure providers are compensated fairly for all services rendered, whether through insurance or tax-based support.