R1 LARNER SPOTLIGHT: Morelli Lab Investigates Therapies for Neurodegenerative Disease
May is awareness month for amyotrophic lateral sclerosis (ALS), a progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord. Also known as motor neuron disease or Lou Gehrig’s disease, ALS is a rare, terminal disorder that causes the progressive loss of voluntary muscle contraction. The Centers for Disease Control estimates the incidence of ALS to be approximately two cases per 100,000 across the U.S. There is no cure for ALS, and the exact cause of the disease is unknown.
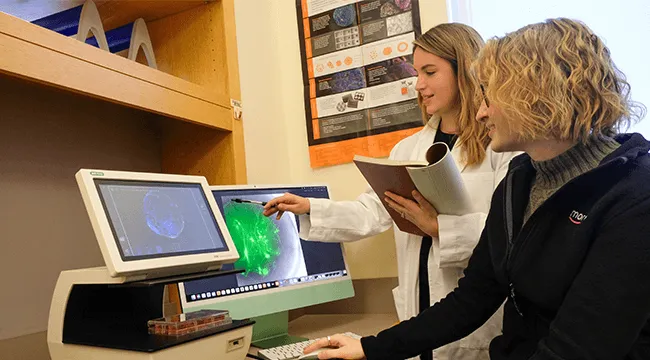
Research by Kathryn Morelli, Ph.D., assistant professor of neurological sciences, seeks to understand how RNA metabolism influences cellular function in neurodegenerative disorders, including ALS. Morelli studies RNA-protein interactions in the brain using advanced RNA-targeting therapies, genomic sequencing, and brain organoids, which are three-dimensional (3D) multicellular tissues derived from stem cells and designed to mimic the human brain. Working closely with Abby Kirch, a Ph.D. student in her lab, Morelli and her team are focused on developing RNA-targeted therapies for ALS.
As Morelli explains, ALS is driven by toxic RNA that disrupts the function of motor neurons, ultimately leading to neurodegeneration. In the quest for effective treatments, understanding the disease at the molecular level and testing new therapies in models that closely mimic human disease are crucial steps.
The ability to access patient-specific stem cell lines is critical to Morelli’s research. Her lab receives stem cells from Target ALS, a nonprofit organization dedicated to breaking down barriers to ALS research to accelerate the discovery of effective treatments. Morelli’s team uses these human-derived stem cells to create brain and spinal cord organoids.
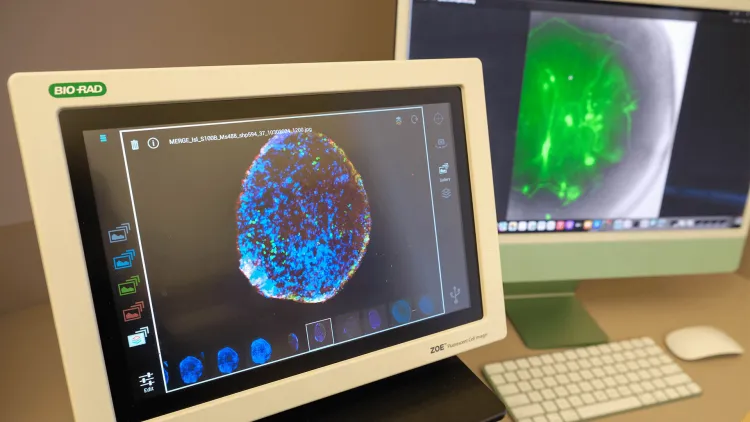
“This has opened so many doors for us because we can make many different types of human preclinical models—patient-specific models—to really look at the molecular etiology of ALS,” Morelli says, adding that the ability to work with these models allows the team to test the efficacy and potential toxicity of new therapies they are developing. “We can evaluate the delivery, efficacy, and potential toxicity of this therapy in human tissue before ever stepping into a clinic,” she says.
Morelli’s research is also supported by the Vermont Center for Cardiovascular and Brain Health (VCCBH), a Phase 1 National Institutes of Health–funded Center of Biomedical Research Excellence that focuses on elevating exceptional early-career faculty. VCCBH provided Morelli with a pilot grant to develop new treatments for frontotemporal dementia (FTD), a rare, progressive brain disease in the frontal and temporal lobes of the brain. This debilitating condition affects behavior, language, and cognitive functions. It is one of the most common dementias to strike younger people, with symptoms starting between age 40–65.
This story was adapted from an article by Target ALS
Research like this has contributed to the University of Vermont’s designation by the Carnegie Classification of Institutions of Higher Education as an R1 institution, placing it in the top tier of research universities in the U.S.