Be it peanuts, bee stings, shellfish, or other triggers, many families live with the day-to-day risk that their child might experience a sudden and scary allergic reaction. In fact, pediatric emergency department visits in the United States to treat acute allergic reactions more than tripled from 2008 to 2016.
But once they arrive at the hospital, many children are staying much longer than necessary, according to a study involving more than 5,000 children conducted at 31 hospitals in the U.S. and Canada. Findings were published June 10, 2025, in Lancet: Child and Adolescent Health.
“This study is important for improving quality of care, hospital operations, and health care resources,” says study co-author Christian D. Pulcini, M.D., M.Ed., M.P.H., assistant professor of emergency medicine at the Larner College of Medicine and attending physician at the UVM Children’s Hospital. “In the past, we used to unnecessarily admit children adequately treated for anaphylaxis to the hospital. The recommendations currently now range from four to six hours of observation after epinephrine. Our study suggests that most children can be discharged safely after two hours of observation.”
Why so much observation time?
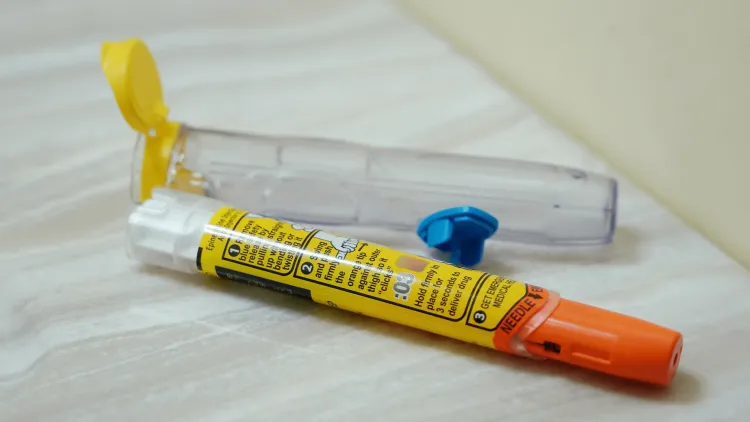
The overwhelming majority of children visiting emergency departments for acute allergic reactions can be routinely treated and promptly sent home. In an age where many people with allergies—even young children—carry their own epinephrine injector pens, many situations require no hospital visit at all. However, about 5 percent of children experience a “biphasic reaction,” which means their symptoms can return even though they received an epinephrine injection. In the absence of clear standards, many clinicians choose to keep patients in hospital for long periods of observation just in case.
“One concern about biphasic reactions is that the time it takes for symptoms to re-emerge can be highly variable,” says Timothy Dribin, M.D., an emergency medicine physician at Cincinnati Children’s. “This study was designed to take a closer look at this population and determine if children at very low risk can be better identified and discharged safely.”
Clearing the backup
The research team gathered data from 5,641 emergency department visits where anaphylaxis was treated with an epinephrine injection. About 90 percent of the children who were studied experienced allergic reactions to foods, including peanuts, eggs, milk, shellfish, sesame, gluten, and soy. In some cases, the exact food trigger was not known. About 6 percent involved medication reactions and 3 percent involved insect stings.
While nearly 17 percent of children were admitted for overnight observation and others stayed in emergency departments well beyond four hours, the need for second doses of epinephrine to cope with biphasic reactions tended to show up quickly. The study found that 4.7 percent of patients received a second dose within two hours of their initial injection and that 1.9 percent received a second dose after four hours.
Some children clearly needed hospital-level care from the moment they arrived at the hospital. About 1 percent of all the children studied needed high-acuity services, such as ventilators to support breathing. But among the rest of those admitted to hospital beds, most never needed a second epinephrine shot, much less intensive care.
“We stratified the patients by severity groups and found that patients with no cardiovascular involvement were at low risk of receiving repeat epinephrine beyond two hours after the initial epinephrine dose,” Dribin says. “Meanwhile, even the patients with cardiovascular involvement were at low risk of receiving repeat epinephrine beyond four hours.”
Potential time and resource savings
Having beds occupied for any unnecessary observation periods makes it harder to serve other patients in need. Emergency departments can get crowded quite quickly, and overcrowding is a known issue in Vermont. This study’s findings can help alleviate overcrowding for children and families who no longer need to remain in the hospital.
“An important value of this study is that it was large enough that the results can give clinicians confidence that discharging patients showing no concerning symptoms in less than two hours is going to be safe for most children,” says David Schnadower, M.D., M.P.H., director of the Division of Emergency Medicine at Cincinnati Children’s.
The study did not attempt to calculate the potential cost savings that could be achieved because hospital prices and care practices can vary so widely. However, the savings from reducing unnecessary hospital admissions could be substantial, the co-authors say. Having the choice to leave the hospital can also be empowering for families who feel comfortable managing at home.
“Families and providers together now have more options in terms of safe observation periods after epinephrine is administered for anaphylaxis in children,” Pulcini says. “Shared decision-making with families is important.”
“We also have seen patients and their families avoid or delay going to the emergency department because they didn’t want to sit there for hours of observation,” says co-author Hugh Sampson, M.D., an allergist at the Icahn School of Medicine at Mount Sinai in New York City. “Such delays can prove dangerous. This study’s findings support discharging patients more expeditiously, which will likely reduce patient reluctance to seek necessary help.”
Funding sources for this study included the National Center for Advancing Translational Sciences and the National Institute of Allergy and Infectious Diseases.
Research like this has contributed to the University of Vermont’s designation by the Carnegie Classification of Institutions of Higher Education as an R1 institution, placing it in the top tier of research universities in the U.S.

