Sometimes called “silent and silenced,” Chagas is a neglected tropical disease that infects seven million people in Mexico, Central America, and South America—and is spreading to other parts of the world. Most don’t know they’re carrying the parasite that causes Chagas. But, years later, intestinal illnesses, chronic heart problems, and death can result. Researcher Lori Stevens and her students are part of an international team fighting back with high-tech insights from UVM labs—and low-tech solutions in communities in Guatemala and other parts of Central America. They’re succeeding. Their work begins with the recognition that promoting public health must go far beyond studying a parasite or any single disease—to a deep understanding of how people, landscapes, animals, economies, and knowledge weave together. “Really,” says Stevens, “there’s only one health.”
With a curved pair of tweezers, Lori Stevens picks up a miserable bug. The insect itself is not miserable—it’s dead and just came out of a freezer in Stevens' lab on the third floor of Marsh Life Science. In the sunlight, the tan-and-black checkered pattern around the edge of its flattened abdomen glints as Stevens turns it upside down. It’s a kissing bug, a member of a blood-sucking group called triatomines. When people sleep, these creatures come out from the darkness and feed, “kissing” them, often with painless bites around the mouth. As the bug’s abdomen fills with blood, it’s obliged to defecate. Sometimes these liquid feces—bug poops—fall into the wound or get into a person’s eye. From there, they can transmit a microscopic parasite, Trypanosoma cruzi, that causes Chagas disease. It’s a cryptic and much neglected malady that brings misery and ill-health to millions of people across Latin America—and 12,000 deaths there each year, far more than malaria. A miserable bug.
Stevens—a professor in UVM’s Biology department since 1988—has been part of an international team of scientists and public health workers trying to stomp on Chagas disease. They’re having remarkable success in Guatemala, combining sophisticated laboratory insights about the genetics and ecology of kissing bugs with low-cost, community-based approaches to making houses “refractory,” as the scientists say: keeping the bugs out of people’s homes.
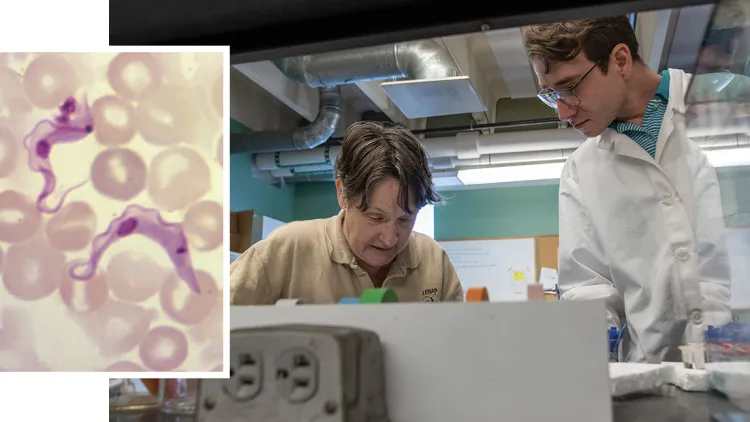
A pair of Trypanosome Cruz parasites visible in a blood sample at 1200X magnification. Right: Professor Lori Stevens and UVM doctoral student Daniel Penados–a citizen of Guatemala– work together to extract and study a complex mash of DNA in the abdomen of kissing bugs.
In the lab, a few minutes later, Daniel Penados holds up a vial with just the abdomen of a kissing bug floating in alcohol. “Should we crush this one?” he asks Stevens. “Crush your heart out!” she says with a laugh. But, actually, he’s going to crush the DNA out. And inside that DNA is a world of information about what the kissing bugs have been eating, which, in turn, has allowed the team to unravel several mysteries about how to break the transmission of Chagas disease.
Chagas is, mostly, a disease of poverty. In Guatemala, many houses are built with adobe bricks or with bajareque, a traditional material made from a lattice of sticks covered with mud. Dirt floors are common. If they’re not maintained to prevent cracks and openings, these materials make perfect habitat for kissing bugs. Like the forested crevices and caves they naturally inhabit, the bugs can hide there during the day. And many poor people bring their dogs, chickens or other livestock into their homes—which also attracts these blood-feeding insects.
Daniel Penados has seen this up close. He’s from Guatemala—now a UVM Ph.D. student doing research with Stevens and biology professor Bryan Ballif. Penados started working on Chagas with Stevens in 2019 when he was still an undergraduate at the University of San Carlos in Guatemala City. (Fun fact: the University of San Carlos was founded in 1676.) His mentor in Guatemala, professor and entomologist Carlota Monroy, has been a pioneer in studying and attacking Chagas disease since the 1980s. She’s part of a trio of senior women scientists leading this research effort, in addition to Stevens and their colleague Patricia Dorn, a distinguished biologist at Loyola University in New Orleans. It was Monroy who encouraged Penados to come to Vermont, part of an exchange of undergraduate students between the University of San Carlos and UVM that she and Stevens arranged with support from the National Science Foundation. “When I started my undergrad, I pretty much didn’t care about Chagas disease,” Penados says. His family runs a successful laboratory testing business in Guatemala City. “I just wanted to learn molecular techniques in the lab. But I ended up loving learning about Chagas, and the communities, and how you are improving people’s lives with this work.” After he graduated, and the pandemic had passed, Penados came back to UVM in the fall of 2022 to begin his doctoral research in neurobiology. (And to learn how to ski.)
Penados shows Stevens another vial holding a kissing bug abdomen. Stevens examines the label. “This is the one that we did that paper on, right?” she says. “Let’s save it for the mass spec.”
Two technologies have revolutionized biological research over the last few decades—one is called “PCR,” which is shorthand for the mouthful “polyermase chain reaction.” Invented in the 1980s, PCR lets scientists take specific bits of DNA and rapidly reproduce them into billions of identical copies. It’s like a microscopic copier machine on speed. From there scientists can use the amplified DNA to find genes and ask questions about the genetics of many kinds of organisms. The famed Human Genome Project was built on PCR.
The other is mass spectrometry, or “mass spec” as it’s known in scientist slang. These machines, basically—very basically!—are a ray gun for looking at chemicals. In a mass spec, materials—like, say, bits of blood from the abdomen of a kissing bug—are ionized: bombarded with a beam of electrons that breaks them into positively charged fragments. These fragments are whizzed through an electric or magnetic field, which deflects them toward a detector. The amount these tiny pieces deflect is determined by how much they weigh—by their mass. The pattern they make on the detector—the spectra—can reveal what’s in the sample. Mass spec has been used in a vast array of scientific fields—including fishing out different types of proteins from cells. Like hemoglobin, an animal protein within red blood cells found in the guts of a kissing bug.
Stevens has helped the research team make fundamental breakthroughs in understanding Chagas disease—by developing new approaches with both PCR and mass spectrometry.

Professor and entomologist Carlota Conroy (left) talks with Guatemalan villagers as part of her decades-long quest to help the people of her country understand and fight Chagas. About one-third of people who contract the disease will suffer heart damage that becomes apparent only many years later as progressive heart failure or sudden death.
But to better understand her innovations, it may be helpful to travel back maybe eight million years to South America. There, the microscopic ancestors of the T. cruzi parasite were probably introduced to ground-dwelling mammals by bats—perhaps when some bat-biting insects started also feeding on some unlucky opossums, according to a review study in Parasites & Vectors. By the time the first people had walked over the Bering land bridge (or did they come by boat?) and down to South America, Chagas disease was already well established in the Andes. It may have been transmitted to humans when they made their first settlements near the coast of the Atacama Desert in what is now southern Peru and northern Chile. The oldest-known T. cruzi infection in a human was found in a 9,000-year-old mummy made by the Chinchorro people of that region. (Fun fact #2: it was identified using PCR.)
There are more than 130 species of triatomines—kissing bugs—that transmit the T. cruzi parasites to a wide range of wild and domestic mammals. And there are at least seven strains of the parasite itself, each with its own special forms of infection. Taking a deep-time, ecological view makes clear why Chagas disease will never be eradicated. And it makes clear that knowing which species of kissing bug you have on the end of your tweezers—and whether it feeds on people and where in the world (or house, or forest, or neighboring village) it came from—could make a great deal of difference. “You need to know what you're working with,” Patricia Dorn says, “if you want to control it.”
Which bring us back to Lori Stevens in her laboratory. On this winter afternoon, she’s got Daniel Penados working on her right—and another Daniel, Danny Sanchez—UVM Class of 2026, a Yankees-loving freshman intern—helping her sort vials of kissing bug abdomens on her left. She’s involved dozens of graduate and undergraduate students in her Chagas disease research since she was contacted by Dorn in 2007 about helping Monroy in Guatemala. Stevens is an expert on population genetics—and in those years she was studying Chagas in Bolivia. Monroy, an expert field scientist, was trying to distinguish strains of the kissing bug species Triatoma dimidiata—the most important carrier of the T. cruzi parasite in Central America. Based on the bug’s body features, like color and shape, it was very difficult to distinguish the strains. “That's why Lori started to work with me,” Monroy says. “To understand the difference between one T. dimidiata strain—from the other, the other, and the other. Which ones transmit the disease in the houses, and in the field, and which ones transmit the disease in the forests?” Stevens was able to help distinguish them genetically—using PCR-based lab techniques.

Danny Sanchez, a first-year undergrad from the Bronx, helps in Lori Stevens’ lab. “I’d never heard of Chagas disease or kissing bugs. I’ve never been out of the country and I’m learning a lot here,” says Sanchez, the first in the family to go to college. “I needed an extra credit and I found that research was interesting. So my advisor was like, ‘I know a researcher. She’s really good.’ And that’s how I started working for Lori.”
In 1915, some kissing bugs from Venezuela—in the species Rhodnius prolixus—accidentally escaped from a research laboratory in San Salvador, the capital of El Salvador. They spread through Central America, forming domesticated populations in buildings, often in the palm leaves used as roofing. They were dangerously effective carriers of Chagas, dropping feces down from the roof into people’s food. A massive spraying campaign of insecticides, begun in the 1960s, has been successful in knocking back R. prolixus in many houses in South America. By 2008, insecticides had also successfully stopped transmission of Chagas by R. prolixus in Guatemala and throughout most of Central America.
But the kissing bug native to Guatemala—Triatoma dimidiata—is a different critter. These bugs will frequently reinfest a house soon after pesticide spraying. Repeated applications are too expensive for many communities in Guatemala and throughout the region. More important, pesticides are nasty, causing environmental and human health problems. (Plus they run the risk of triggering the evolution of pesticide-resistant populations, as has been seen in a South American kissing bug species, Triatoma infestans.)
So why do these T. dimidiata kissing bugs keep coming back into people’s houses? Over the last two decades, the research team led by Monroy, Dorn, and Stevens has unraveled the mystery of rapid reinfestation—and what to do about it. The short answer: some of these bugs move—a lot—happily jumping from house to house, or from nearby forests and woodpiles. So it’s better to keep them out—rather than try to kill them in.
In a 2022 review paper, the team describes one of their experiments where houses in a Guatemalan village were treated with pesticides. Less than two years later, a third of these houses were reinfested with kissing bugs. That study—developed in collaboration with UVM professors Sarah Helms Cahan in the Biology Department and Donna Rizzo in the Department of Civil and Environmental Engineering—and others like it, relied on advanced PCR techniques looking at sections of DNA with astounding names like single nucleotide polymorphisms, microsatellites, and random amplified polymorphic markers. (Fun fact #3: these are really cool and complicated techniques that you can read about on your own time; we’re moving on with the bug story.) And that story, revealed in the DNA, showed that the kissing bugs in many houses, and even in villages 60 miles apart, are closely related—meaning they must be highly mobile.
“Pesticide has been effective in South America because there is a species that is only living inside the house,” Monroy says. “But, in Guatemala, Triatoma dimidiata is not only living inside the houses. It’s all over and its movement makes it very difficult to control only with pesticide. That's why I decided to work with non-traditional ways of control many years ago—we needed a new method.”
That method has come to be called an “EcoHealth” approach (or, increasingly, “One Health”). “It begins with the people, my people,” says Monroy, who has been able to build connections between Guatemalan citizens, community leaders, researchers, and Ministry of Health officials and field workers. “Nothing will work without the local community making it work,” she said. So the researchers reached out to two villages in southern Guatemala, La Brea and El Tule—both highly infested with kissing bugs despite regular insecticide spraying by the Ministry of Health. They began working with residents to make improvements—that local people already wanted. “We learned that wall plastering was the most common house improvement undertaken; traditionally, women, using their hands, plaster the walls to beautify the house,” the team writes in Frontiers in Tropical Disease. Mud was customary, but easily cracked, quickly opening places for kissing bugs to hide. So local leaders worked with Monroy, others on the research team, and architects and engineers to formulate an improved plaster using low-cost, local ingredients, including sand and volcanic ash, designed to be resistant to cracking. They also formulated a cement-like material for making poured floors, using volcanic ash and lime at one-tenth the cost of commercial cement.
And then young men from the village were hired to instruct and help residents make their own improvements. “People like having bright, clean walls and solid floors,” says Dorn, so their bug-blocking benefits don’t cut against the culture. With these in place, residents were supplied with chicken wire to make their own chicken coops, getting the birds out of houses. Finally, the householders were provided with fruit trees to replace trees harvested for chicken coops. These trees can provide improved nutrition and a market opportunity for selling fruit—and also promote reforestation, since one force pushing Guatemalan kissing bugs into human habitat is destruction of their forest habitat.
Monitoring these changes from 2001 to 2020, the team has proven they have many benefits. For example, “we've documented that by moving the chickens to an outdoor coop, they’re raising a lot more chickens. And women control the chickens and the sale of chickens and the eggs. And so women are better off now,” Dorn says. “And, of course, they cook them for dinner—everybody's eating more protein.”

At night, both nymphs and adult kissing bugs come out to feed on people as they sleep. Researchers and public health workers search for the insects to collect and study them at LENAP, the Laboratory of Applied Entomology and Parasitology at the University of San Carlos, and in biology labs at the University of Vermont.
In the two test villages with house improvements, the levels of kissing bug infestation plummeted, falling below an 8% threshold, where transmission of Chagas becomes unlikely. But to show that the EcoHealth approach actually works—and to convince the Guatemalan Ministry of Health—the scientists needed to prove not only that the houses kept out the kissing bugs over the long term—but also that people were not contracting the parasite.
And that, again, brings us back to Lori Stevens in her laboratory, where, on this winter afternoon, she is patiently explaining to a visiting science reporter what PCR primers are and why they matter—and how they relate to dog chow. Years ago, she had heard that PCR was being used to detect contamination in dog food. “Companies would say it was all pork—but then people would amplify DNA samples to find chicken and beef,” Stevens says. And that got her thinking: “When you take off the end of the bug—you've got DNA of the parasite, DNA of the bug, DNA of any microbiome, and DNA of the blood meals in there,” she says. Stevens put her skills to work and developed tools to extract this jumble of DNA from the abdomen of the kissing bugs and then designed custom primers—specialized short single strands of DNA—that could be used to “amplify human DNA, dog DNA, mouse DNA, chicken DNA, and so on,” Stevens explains, “so that we could look and see what the bugs were feeding on.”
This innovation by Stevens was followed by another that she and Bryan Ballif and others developed with mass spec. Stevens had heard that researchers were studying mosquitoes by looking for a distinctive signature of different species in their hemoglobin. She and Ballif developed a way to do the same with kissing bugs—finding hemoglobin signals from the many animals they feed on. These proteins are less prone to falling apart than DNA and last longer, so they have been able to provide a highly accurate confirmation of the results from PCR—and a high-resolution picture of a kissing bug’s diet.
With these tools in hand, the Chagas researchers could see that the T. dimidiata kissing bugs were feeding on a range of animals outside the houses (like cows) and people inside the house—as well as moving from house to house. And, critically, they could show that after the EcoHealth improvements, the kissing bugs shifted away from human blood meals, dropping from 40% of bugs found with human DNA to less than 10%.
After launching the EcoHealth approach in these two Guatemalan villages over 20 years ago, the research team took the show on the road, expanding the effort into other landscapes and cultures, surveying villages in Guatemala, El Salvador, and Honduras. And in a region-wide EcoHealth project launched in 2018, with 51 villages in two regions of Guatemala, led by the Ministry of Public Health and numerous other organizations, the scientists report, “no child under five years old was found T. cruzi positive”—indicating that the transmission of Chagas disease was blocked for at least five years.
A recent study by Monroy estimates that 85,000 people that live in Central America are now at much reduced risk of Chagas disease because of the approach she pioneered. She’d like to protect millions more. “The science we do here is important for validating the work of people like Carlota in the field,” says Stevens, sliding another box of kissing bugs out of the freezer. “The genetic data that we've generated at UVM shows how much the bugs move over the landscape. I enjoy thinking about that. It puts these tiny things we study in the lab into a bigger perspective.”