Nuclear Medicine
Introduction to Nuclear Medicine

Lesson Objectives
- Basics of nuclear medicine. How does it differ from the rest of radiology?
- Basics of radioisotopes and how they generate images.
- Basics of nuclear medicine scanners.
- Basic interpretation of nuclear medicine studies.
- Introduction to FDG PET-CT.
- Common clinical applications of nuclear medicine.
- Role of radioisotopes in treatment.
What is Nuclear Medicine?

Nuclear medicine is a unique part of radiology in which it generates images primarily based on physiology and function, therefore images are usually low resolution and have poor anatomic detail.
- Anatomical detail is limited because only the parts of the body that absorb or metabolize the radioisotope will show up in the image.
- Images produced are highly dependent on which radioisotope is used.
Other imaging modalities in radiology focus on anatomy and structure.
- Physiologic function not seen, because these images are based off of relative densities and show you a snapshot of the anatomy.
Radioisotopes

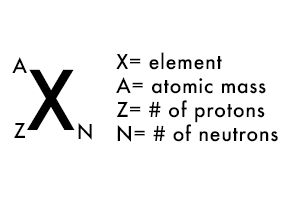
Remember the atom! 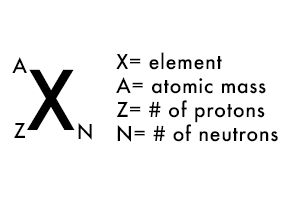
- Atomic number = number of protons in an element.
- Each element may have many different isotopes, which have the same number of protons and differing number of neutrons.
- Radioactive elements constantly undergo decay and in the process emit energy in varying forms.
- Alpha and beta decay = energetic particles are released.
- Photons can be emitted as a form of energy from decay.
- Photons have no mass (i.e. x-rays and gamma rays).
- Photons are used to create images, primarily gamma rays in nuclear medicine.
Examples of Common Radioisotopes
|
Radioisotope
|
Radiation Density
|
Half-life
|
Use
|
|
Technetium-99m
|
Isometric transition
|
6 hours
|
Many uses
|
|
Iodine-123
|
Electron capture
|
13 hours
|
Thyroid imaging
|
|
Iodine-131
|
Beta and gamma emission
|
8 days
|
Thyroid cancer, hyperthyroidism
|
|
Rubidium-82
|
Electron capture
|
76 seconds
|
myocardial perfusion
|
|
Thallium-201
|
Electron capture
|
73 hours
|
Mycardial perfusion
|
|
Fluorine-18
|
Positron emission
|
110 minutes
|
Oncology, myocardial hibernation
|
Nuclear Medicine Scanners
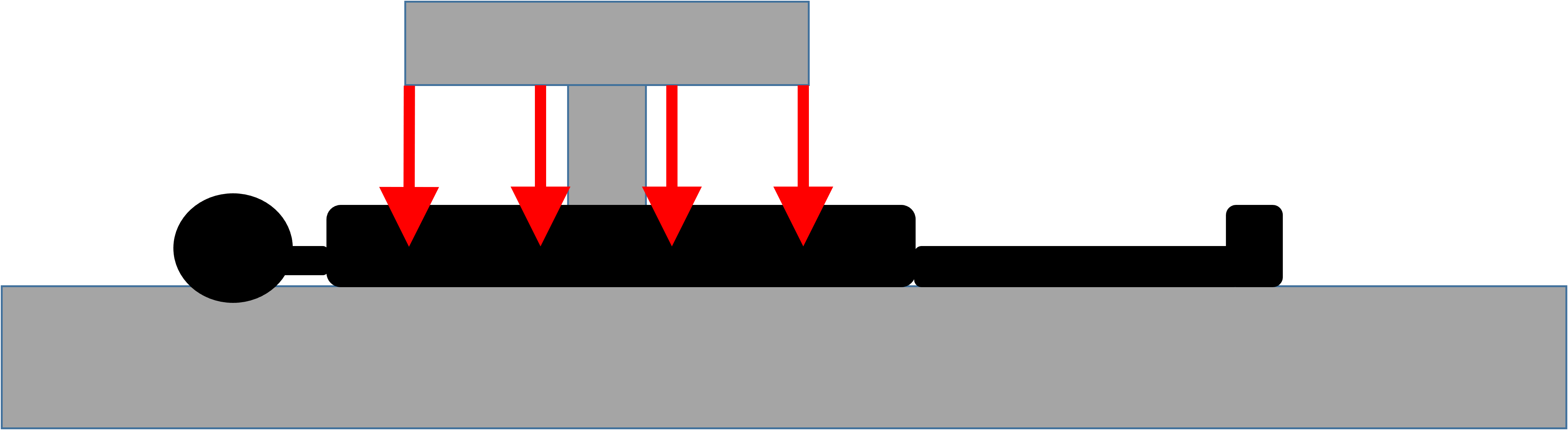
- Nuclear medicine scanners are only detectors that pick up energy emitted from radioisotopes given to patients either orally or intravenously.
- No radiation is emitted from the scanner.
- Scanners count the number of photons and convert the emissions into images.
- In x-ray or CT imaging, radiation is externally generated, passes through the patient, and is captured by the detector on the other side.
- In nuclear imaging, the radioactive isotopes are ingested or injected, and subsequent radiation is internally generated and externally detected as radioactive decay occurs.
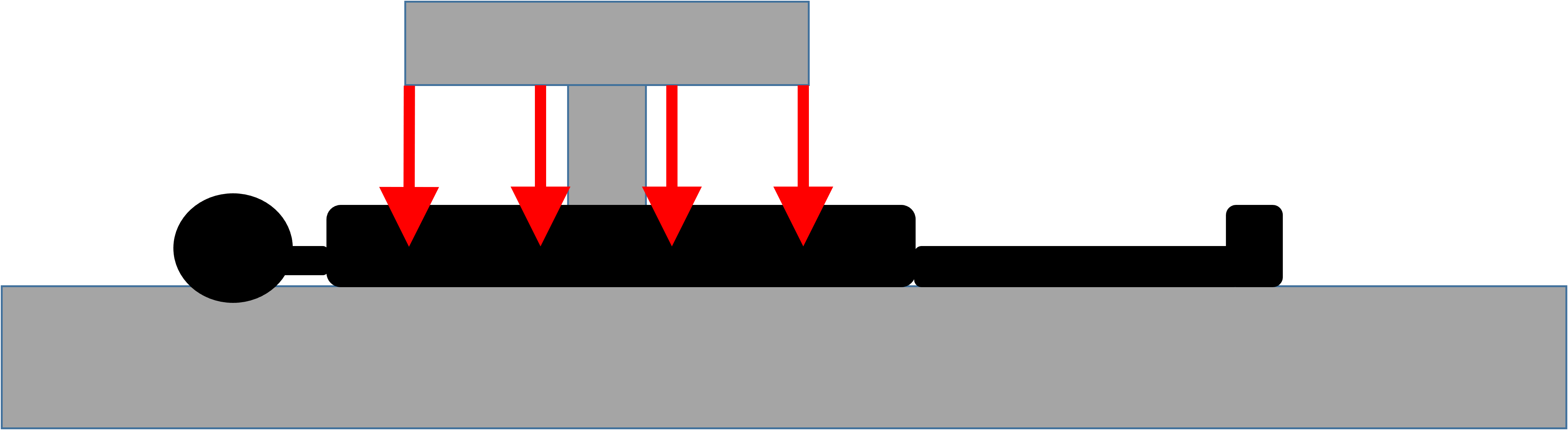

Example of gamma camera
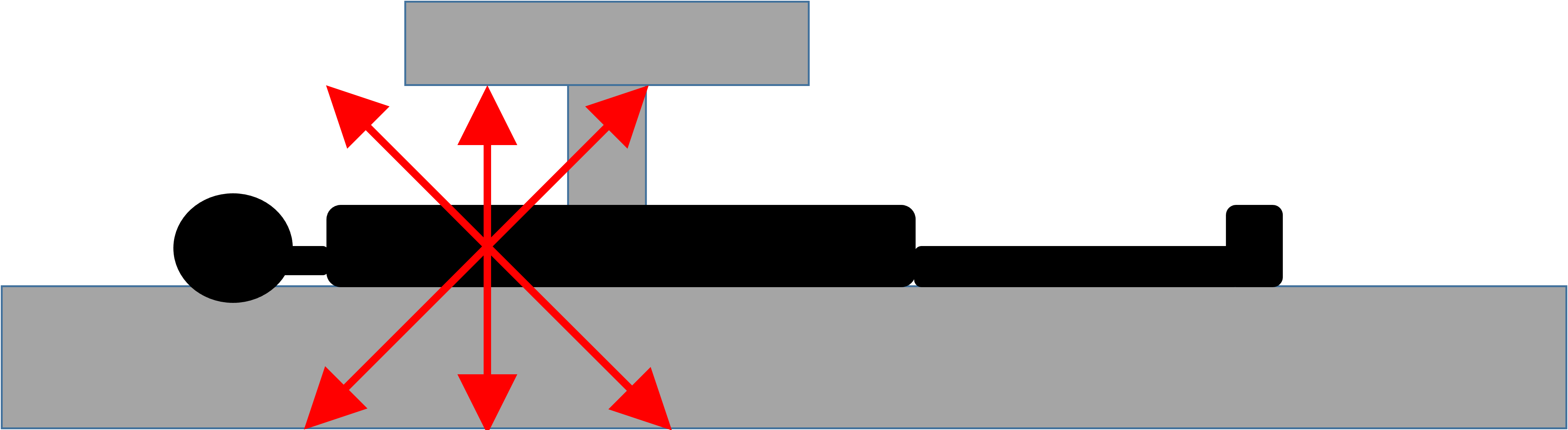
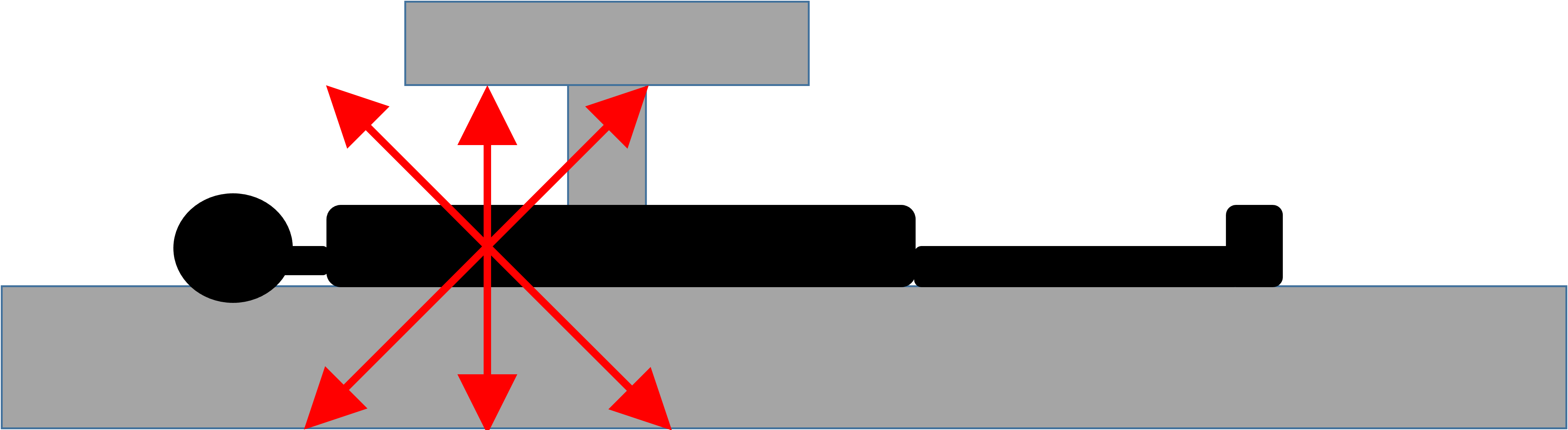
- Positron Emission Topography (PET) scanners are different from gamma cameras.
- They detect positron emitting isotopes.
- Positron = beta particle with positive charge.
- Positron is emitted from the nucleus and after a short distance will collide with an electron, causing an "annihilation" event.
- Annihilation creates two photons traveling in opposite directions which the PET scanner detects and converts into an image.
- PET detector has to detect both photons traveling in opposite directions at nearly the same time for it to be counted.
- PET scanners also include a CT scanner, which can be used to create "fused" images.
Annihilation Event
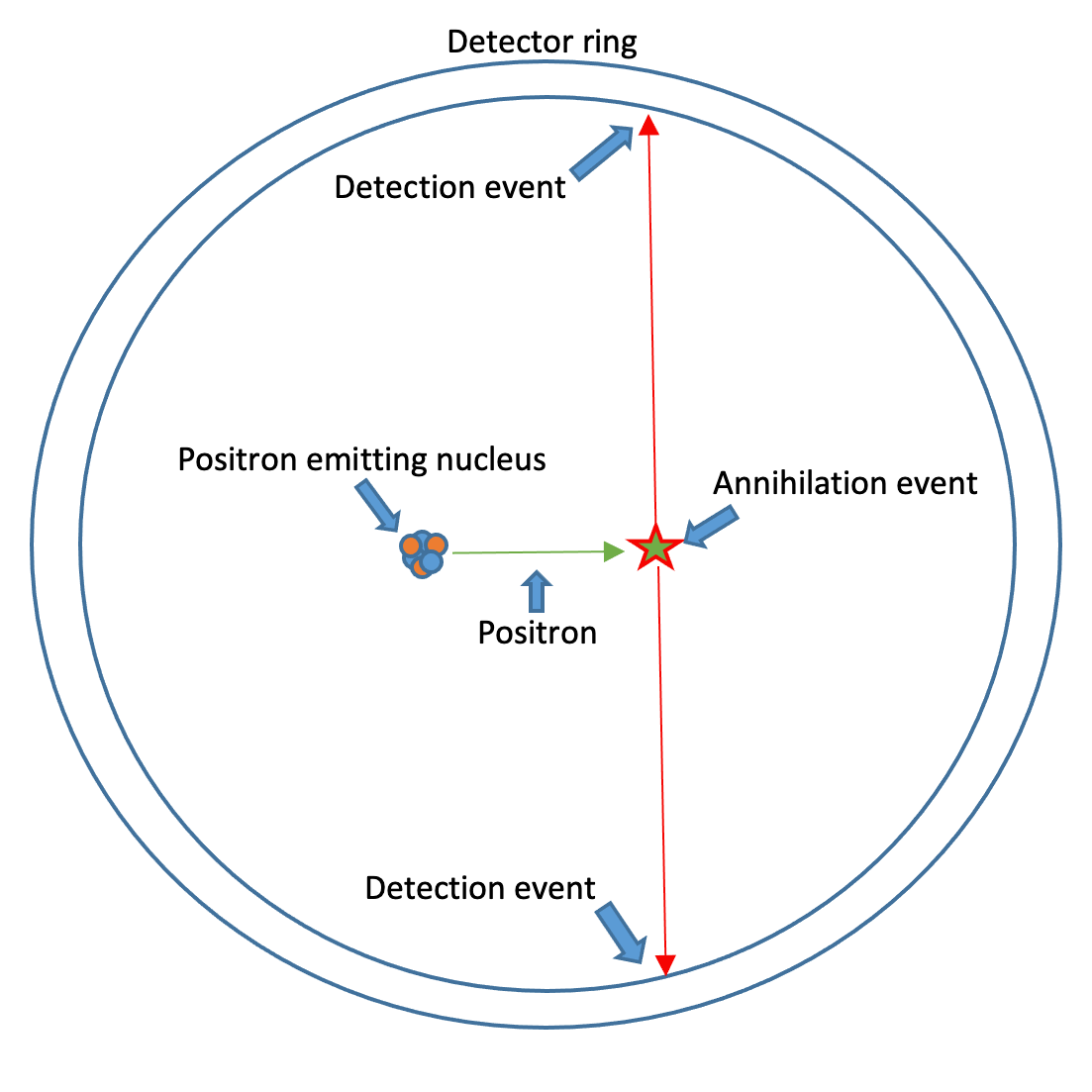
- Positron is emitted from the nucleus.
- Electron and Positron collide, and an annihilation event occurs.
- Two identical photons are generated, traveling in opposite directions.
- Two signals are captured by the detector ring simultaneously.
Interpreting Nuclear Medicine Studies
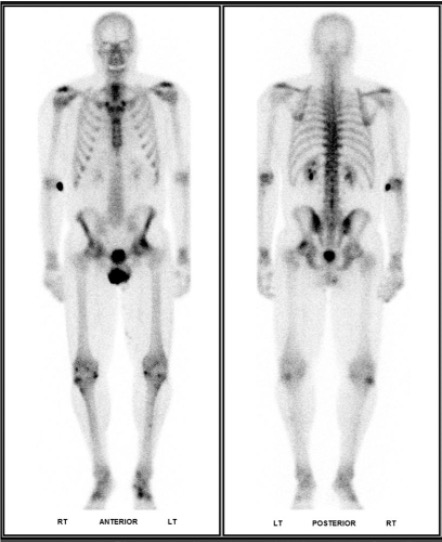
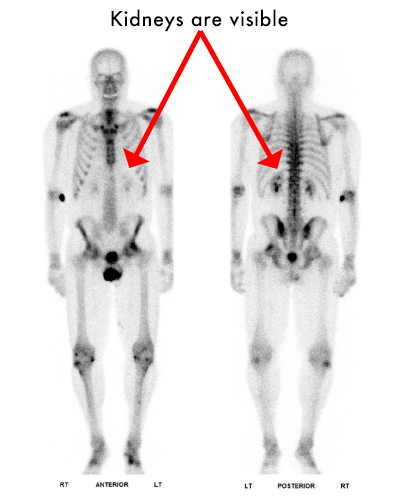
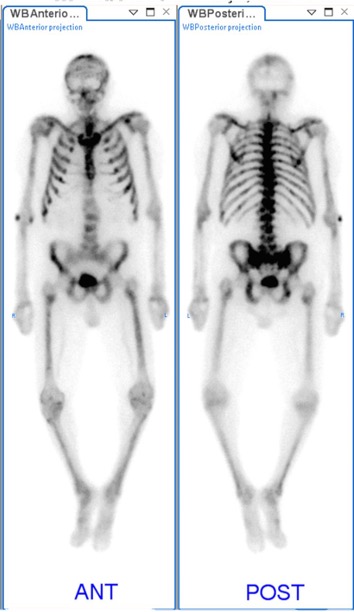
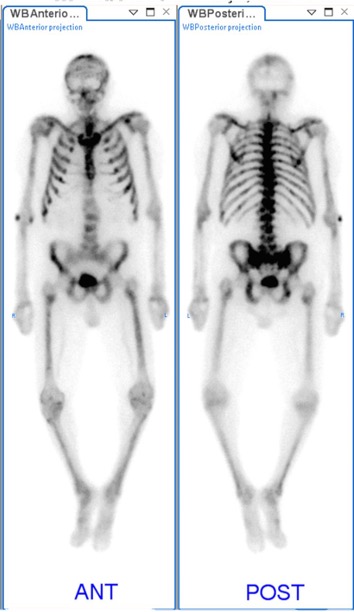
- Most images are in gray scale and have poor anatomic detail, as seen in the image on the right.
- Radioactive isotopes are injected or ingested, and the patient is scanned.
- Photons hitting the detectors are counted and converted into images.
- Black areas represent higher counts, indicating increased radiotracer uptake or "hot" spots.
- White areas represent lower counts, indicating low uptake or "cold" spots.
- In some studies, (such as PET scans) these images can be combined with standard CT scans to create a "fused" image.
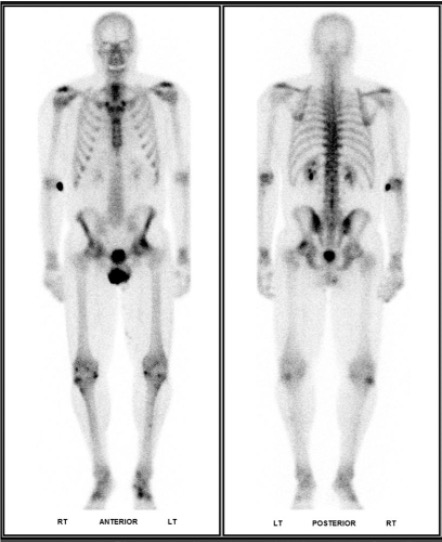
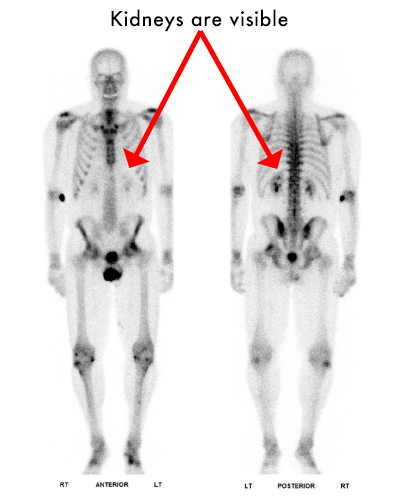
Intro to Bone Scans
- Radiotracer- Technetium 99m MDP.
- "Hot" uptake at sites of active turnover
- Kidneys should be faintly visible. If there is sufficiently strong uptake in the bones, the kidneys will not be seen- this is called a superscan
- Symmetry is your friend!
- Focal uptake in the joints most likely represent degenerative changes.
- If you are not sure- correlate
Test your knowledge
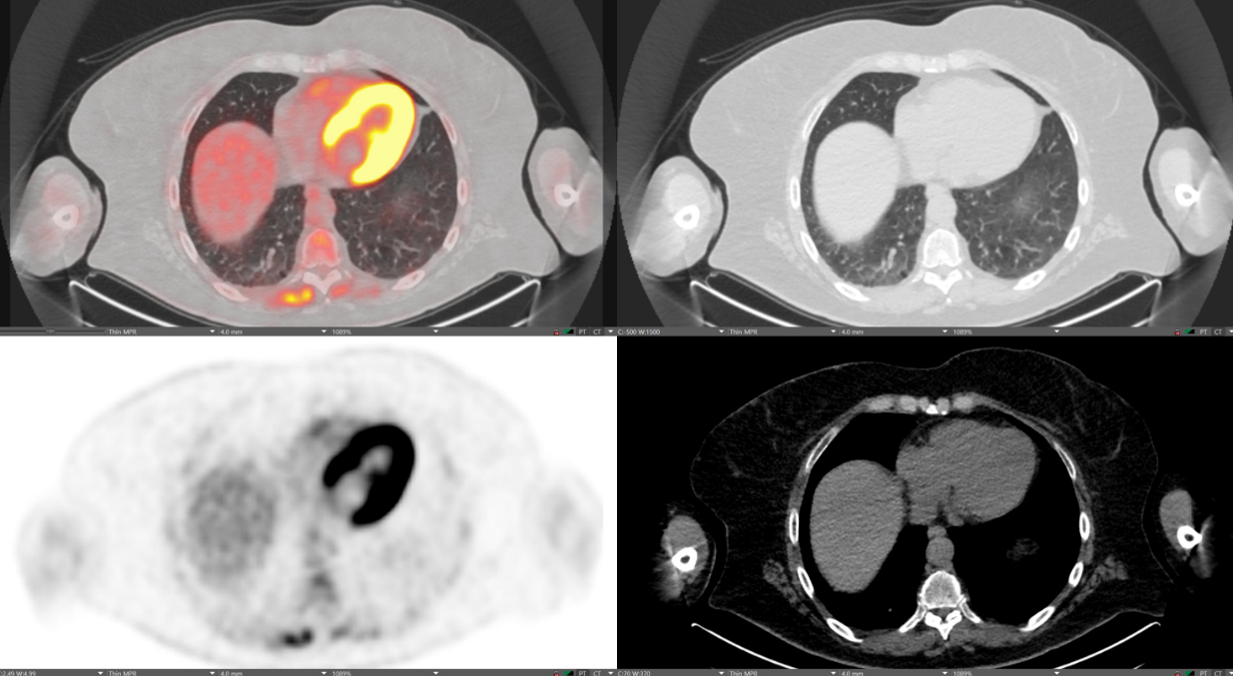
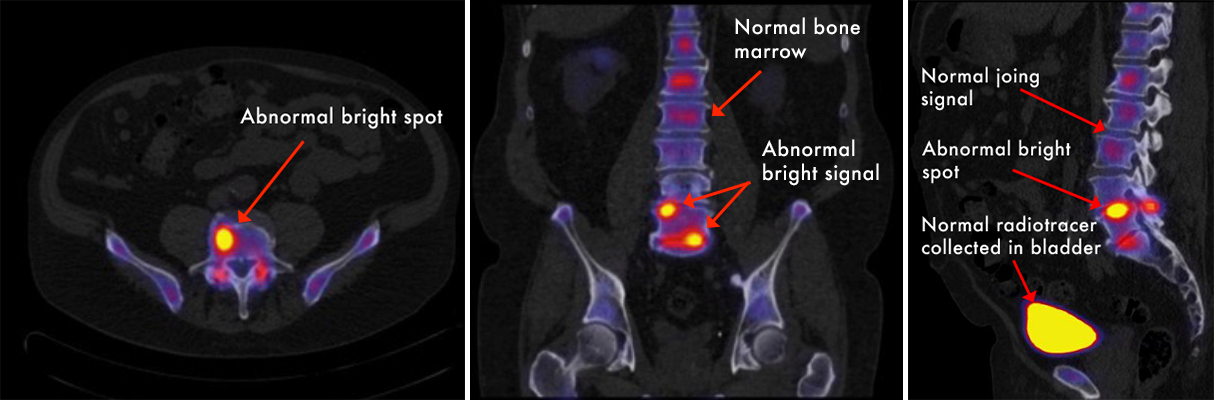
Introduction to PET-CT

- PET-CT is one of the most common studies performed in nuclear medicine with many applications.
- Applications: Assist in staging, treatment response, and monitoring for recurrence for many cancers. Myocardial perfusion testing. Bone scans. And more.
- FDG = fluoro-deoxy glucose, which is made using a radioactive isotope of fluorine (F-18), is one of the most common types of PET-CT scan.
- This simulates glucose metabolism throughout the body.
- A majority of malignancies utilize glucose and will therefore take up the radiotracer.
- CT portion can be fused with the PET image to provide high quality anatomic detail for direct comparison of anatomy and physiology.
- Scanner looks like a normal CT scanner with a built in gamma detector.
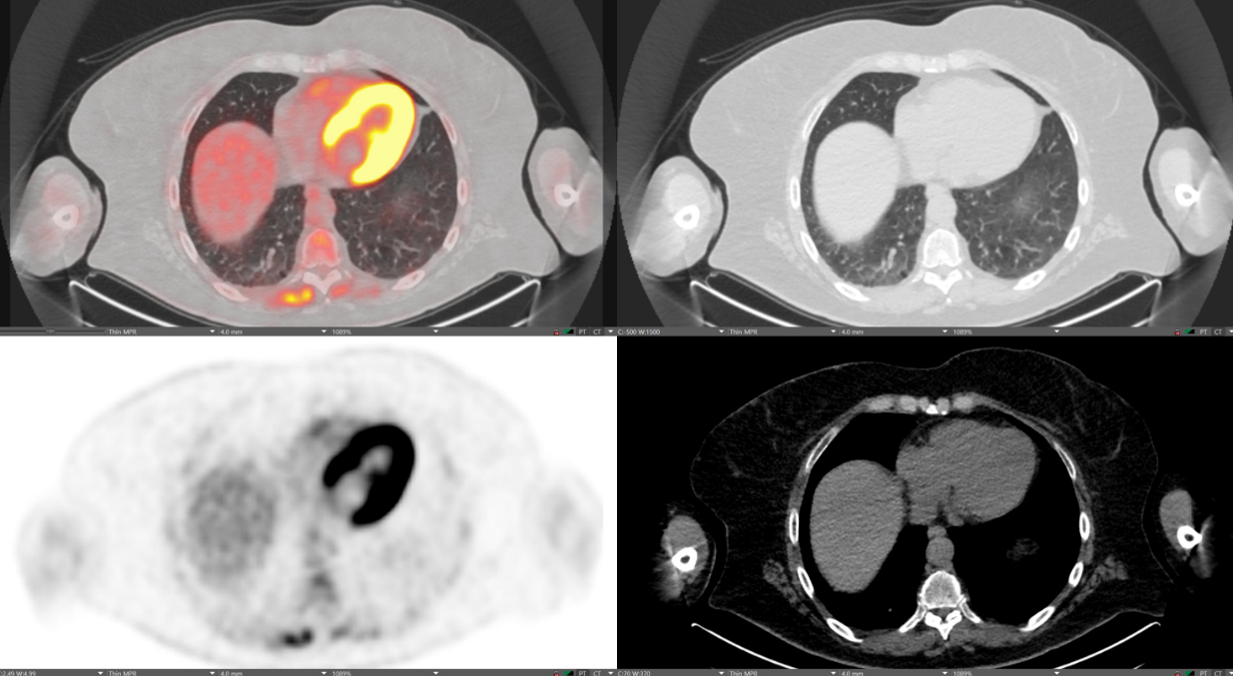
- PET and CT images can be combined to create a "fused" image (see top left image).
- What is considered "normal" depends on which radiotracer is used.
- FDG simulates glucose metabolism- organs that highly metabolize glucose will have a higher signal. For example: heart, brain, bone marrow, kidneys…
- On the right, a "normal" FDG PET-CT shows bright uptake in the highly metabolic myocardium.
- Abnormally high signal where it shouldn't be is a red flag!
- For example- pulmonary nodules are very common on CT and it can be difficult to know how worrisome it is by CT alone. On PET-CT, benign pulmonary nodules have little to no uptake, whereas lung cancer will be very bright.
Test your knowledge

Common Clinical Applications
The following are examples of common clinical applications of nuclear medicine.
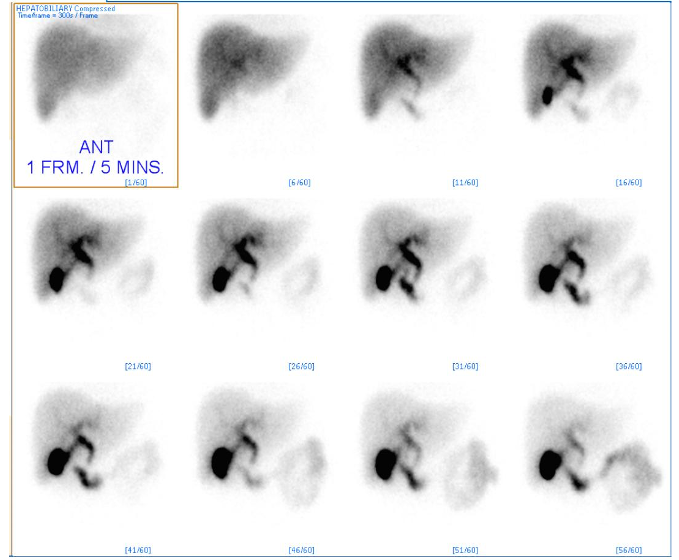
HIDA Scan
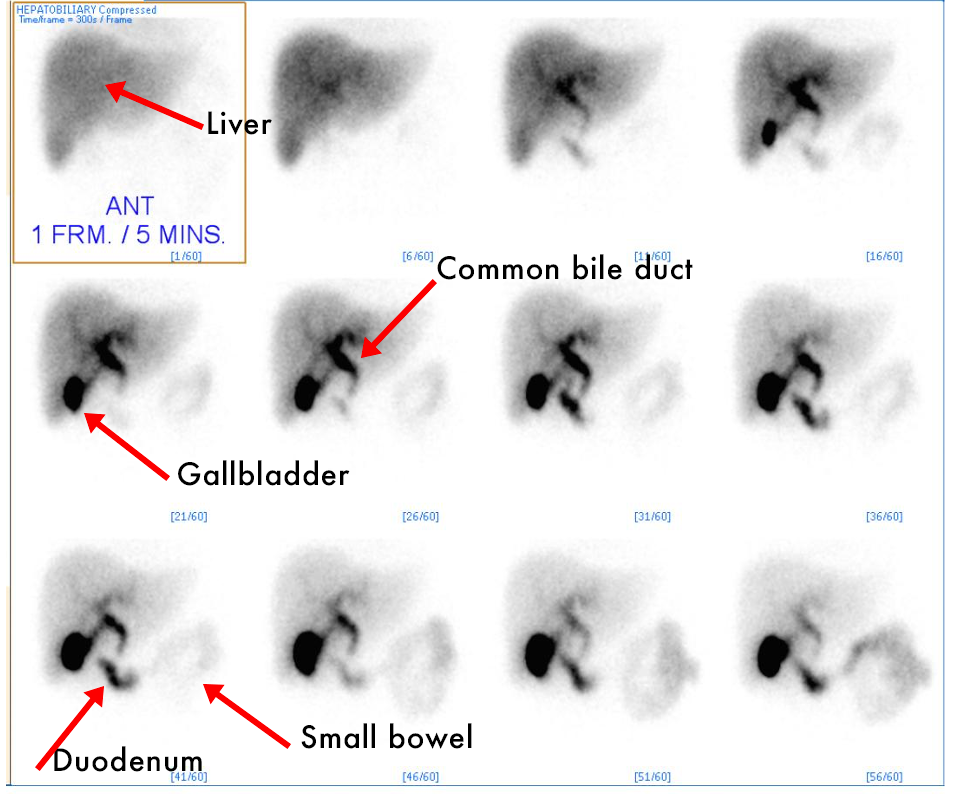
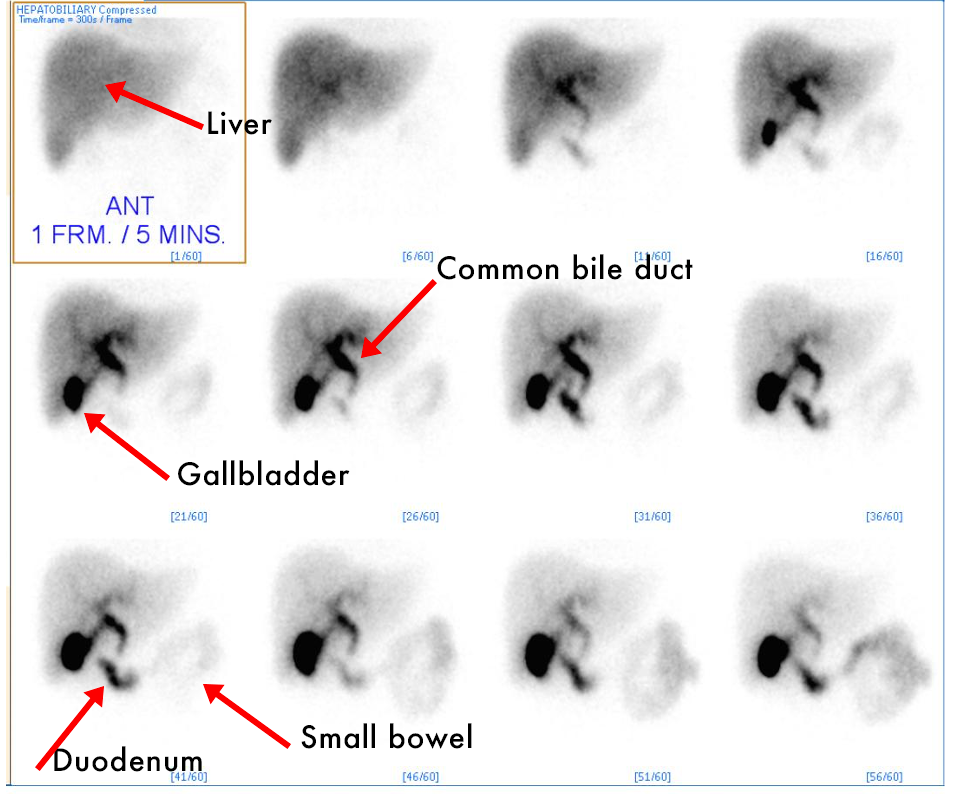
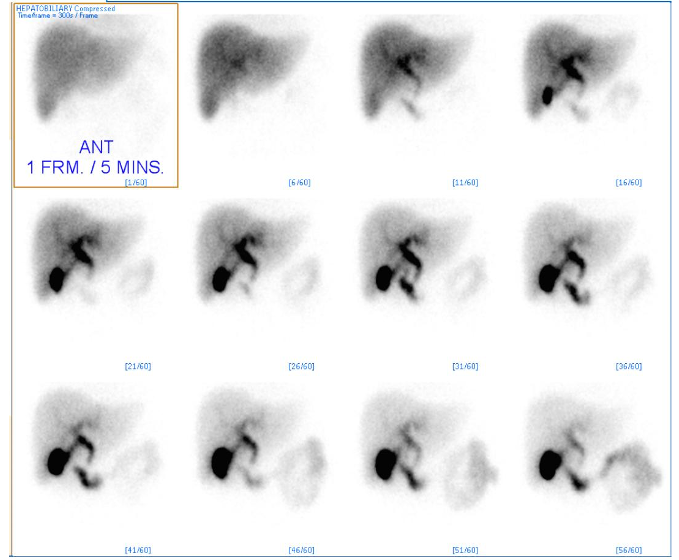
- HIDA (hepatobiliary iminodiacetic acid) scan- Similar to Bone scans, 2D planar images are used to visualize the amount of radiotracer uptake in the biliary tree, specifically the gallbladder.
- Tc-99m Mebrofenin, is taken up by the liver, then excreted into the biliary system where it collects in the gallbladder.
- Over time, it will be excreted via the common bile duct into the duodenum.
Why is this a useful test?
- Acute Cholecystitis: A LACK of radiotracer uptake within the gallbladder.
- Chronic cholecystitis: A gallbladder that fills with radiotracer, but does not empty appropriately after being given an emptying agent.
- Bile Leak: Radiotracer OUTSIDE of the biliary tree shortly following surgical removal of the gallbladder.
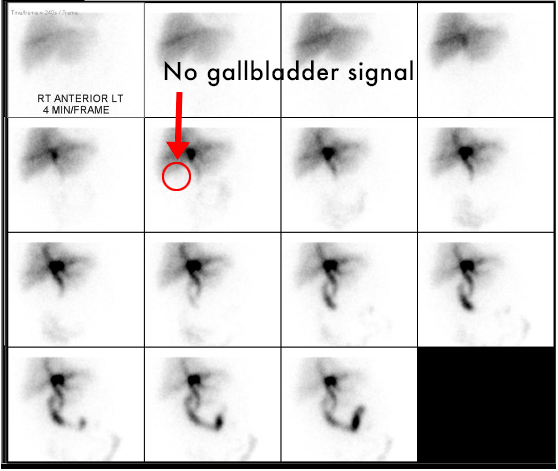
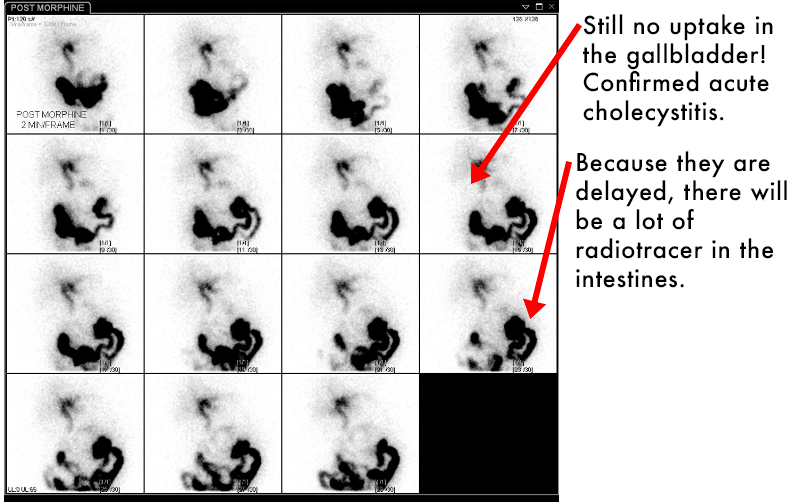
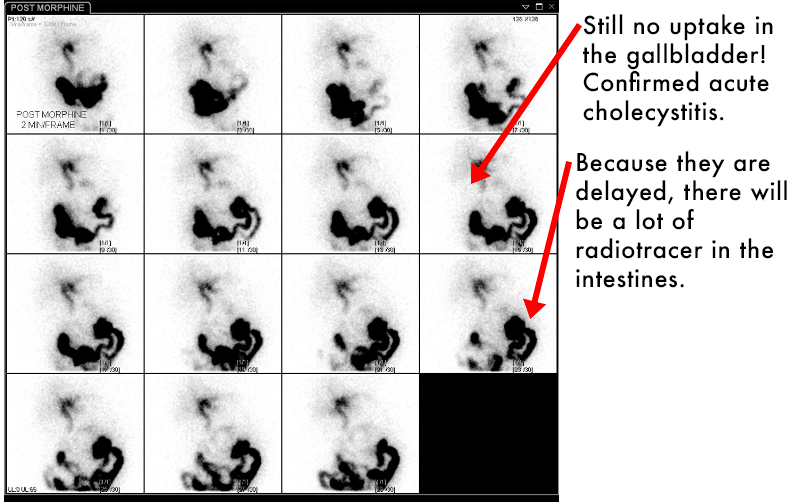
Acute Cholecystitis
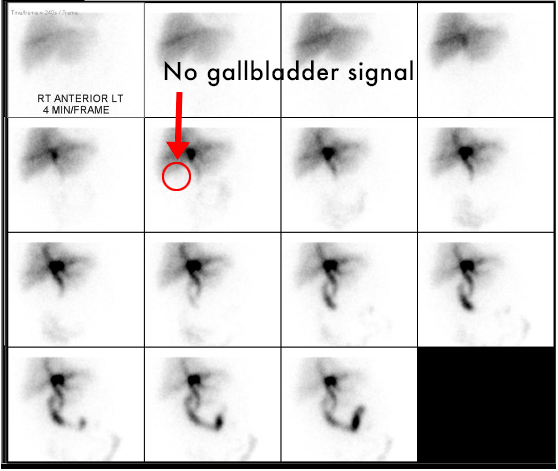
- A normal HIDA scan will demonstrate radiotracer filling the gallbladder, as demonstrated on the previous images.
- In these abnormal images, the radiotracer is visible within the liver, the biliary tree, and the duodenum. However, there is no radiotracer uptake in the gallbladder.
- This is acute cholecystitis! BUT just to be sure (and to avoid unnecessary surgery if it isn't):
- Morphine administration will cause the Sphincter of Oddi to contract (where the common bile duct drains into the duodenum). The increased pressure in the CBD increases the likelihood of radiotracer entering the gallbladder.
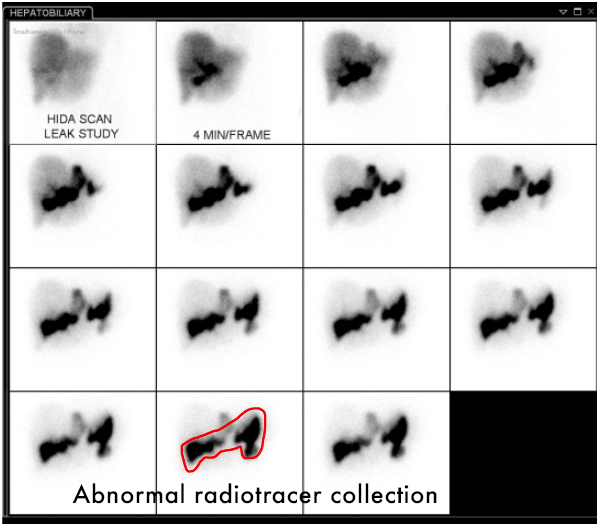
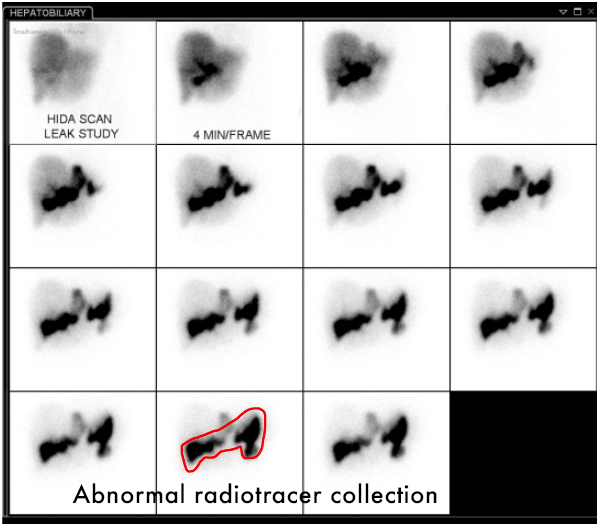
Bile Leak
Shortly after undergoing cholecystectomy, the patient has continued right upper quadrant pain, fevers… The surgeon is concerned about a leak…
- CT scan may or may not give you the answer, because there can be normal postoperative fluid collections that may hide a small bile leak.
- HIDA scan demonstrates radiotracer OUTSIDE of the biliary tree, and not following the course of the intestines.
SPECT-CT - Bone Scan
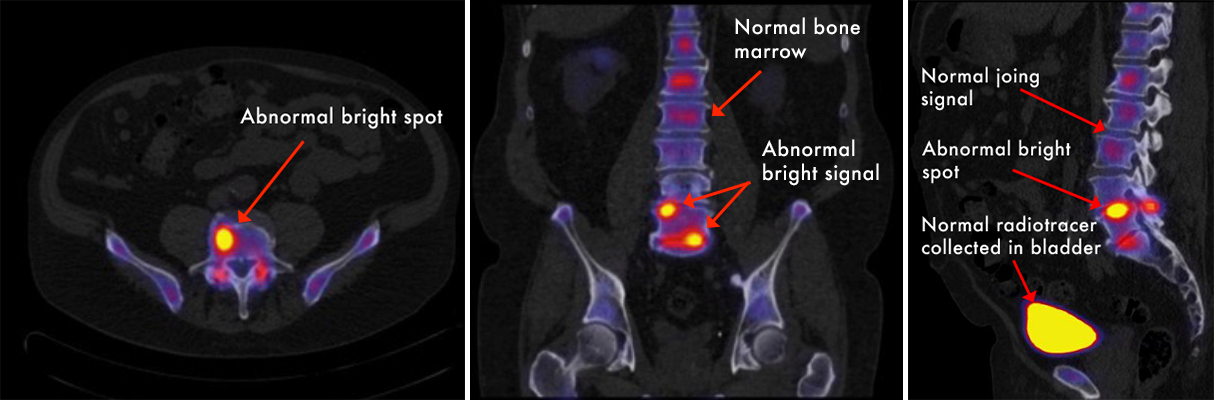
- SPECT = Single Photon Emission Computed Tomography
- Similar in principle to PET-CT, but utilizes different radiotracers to produce gamma rays instead of positrons.
- Primarily used to help target pain injections or guide therapy.
- Combination of CT and nuclear medicine images allow for improved resolution of images and provides anatomical localization.
- Abnormal signal will appear as bright "hot spots," indicating active inflammation and bony remodeling.
- Corresponding abnormalities on the CT images helps us give a more accurate diagnosis.
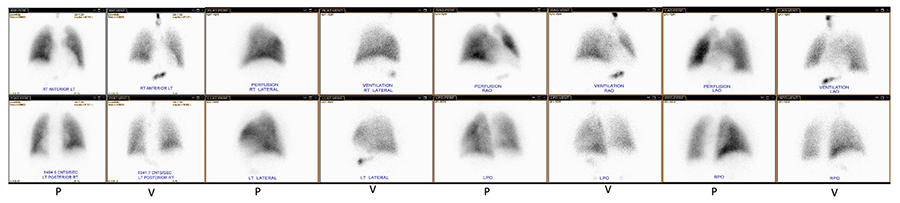
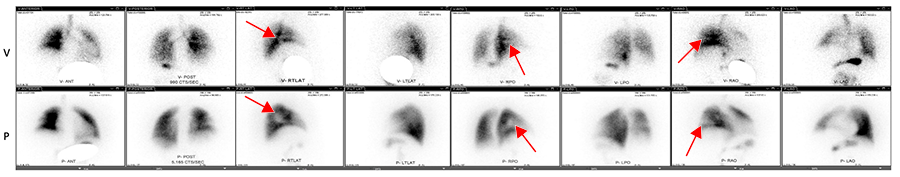
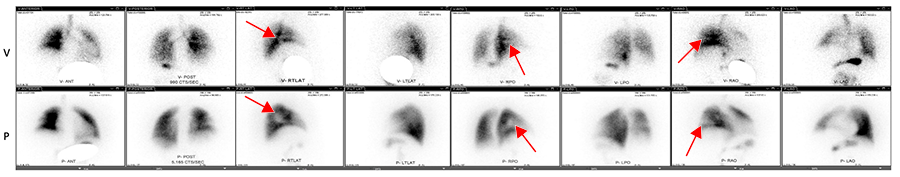
Ventilation/Perfusion Scan (VQ Scan)
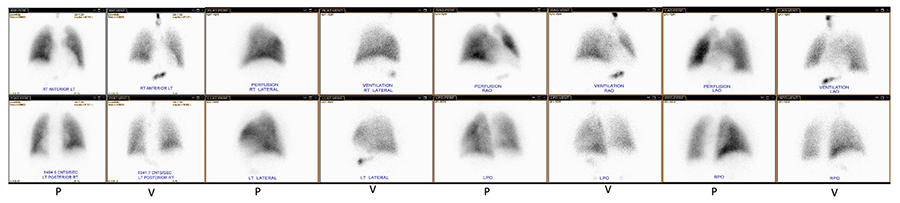
- Two sets of images are taken, with images taken from several different angles:
- The first scan uses inhaled radiotracer particles to demonstrate the airways and any ventilated lung tissue.
- The second scan uses a different injected radiotracer to demonstrate any perfused lung tissue.
- The two scans are compared to look for areas of mismatch. In a case with pulmonary embolism, there would be one or more regions of the lung that are ventilated, but not perfused because the PE is blocking the flow of blood to that area. Look for areas that don't match!
- CAUTION! Always check the labels on the images to see if it a perfusion (P) or ventilation (V) image- they may be organized in rows or columns.
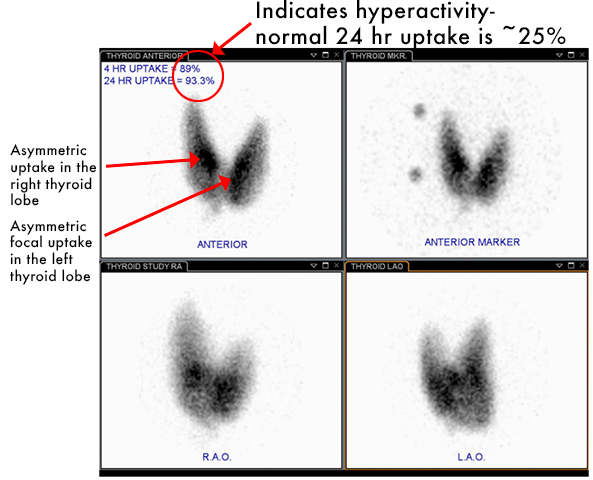
Thyroid imaging: Iodine-123
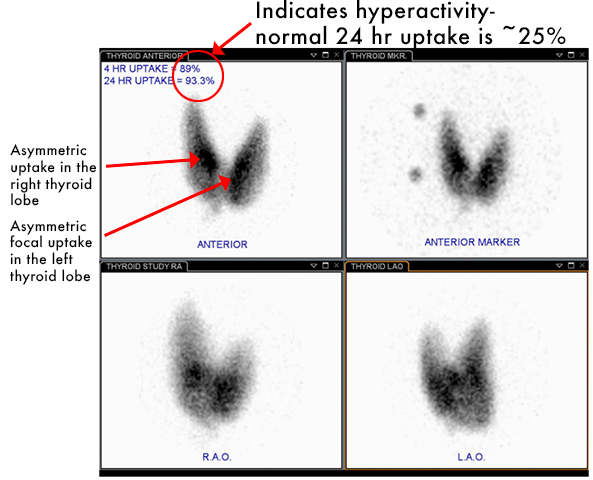
- The thyroid is very efficient at taking up iodine, relative to the rest of the body.
- Because of this, Iodine-123 is ideal for thyroid nuclear imaging.
- Planar images in the thyroid gland are taken at 4hr and 24hr. Normal uptake at 24 hours is typically 15-25% of the administered dose.
-
Why is this useful?
- I-123 scans can determine the degree of thyroid uptake and identify any focal or diffuse abnormal activity. For example...
- Graves Disease: thyroid stimulating immunoglobulin causes diffusely increased uptake.
- Toxic nodule: Asymmetric focal area of increased uptake, indicating a hyperactive nodule.
- Thyroid cancer: a thyroid nodule with a LACK of I-123 uptake is concerning for thyroid cancer.
Role of Radioisotopes in Treatment
I-131 is a radioisotope used for the treatment of thyroid cancer.
- Usually surgery is done prior to I-131 treatment with near total thyroidectomy (parathyroid glands usually preserved).
- Dose is usually given orally.
- Scan after surgery helps localize remnant thyroid tissue or metastases not identified prior to surgery. It also serves to ablate any residual thyroid tissue or any likely remnant metastatic cells.
- I-131 simultaneously images and treats and residual thyroid cancer. TTc