Mammography
Introduction to Mammography

Lesson Objectives
- Basics of mammography.
- Learn about screening mammography.
- How are mammography images obtained?
- Effect of breast density on interpreting mammograms.
- Basics of interpreting mammograms.
- Basics of digital mammography and tomosynthesis.
Basics of Mammography
- A mammogram is a low dose x-ray of the breast used to screen for breast cancer.
- Mammography can also be used in a diagnostic setting such as:
- Further characterize an abnormality seen on a screening mammogram.
- Evaluate a patient or provider's concern found on a self or physical exam.
- Screening mammography is governed by federal law by The Mammography Quality Standards Act (MQSA).
- Set a minimum standard that all hospitals preforming screening mammography must comply to.
- American College of Radiology uses BI-RADS, which standardizes image terminology, report organization, assessment structure and classification system used to risk stratify and help determine next steps in diagnosing and following lesions.
Screening Mammography
- Why screen? About 1 in 8 U.S. women will develop invasive breast cancer in their lifetime.
- Breast cancer has the second highest cancer death rate in women, second to lung carcinoma.
- Early detection of breast cancer can lead to:
- Greater range of treatment options
- Less extensive surgery
- Better treatment outcomes as lower stage cancers have better long term survival.
*Chart (survival, treatment, cost, stage) removed pending source
Regular screening mammography began in the 1980s and the breast cancer death rate has decreased by ~35% since.
Chart accompanying above removed pending source
- Mixed interpretation of the data has resulted in many organizations having different screening guidelines.
- American College of Surgeon (ACS) Guidelines: Age 40-44: Women may begin annual screening, age 45-54: Annual screen, Age 55+: yearly or every 2 years, as long as >10yrs life expectancy.
- United States Preventive Services Task Force (USPSTF): Biennial screening for ages 50-74. Ages 40-49 should be individual choice.
- American College of Radiology (ACR) and American College of Obstetricians and Gynecologists (ACOG): Annual at age 40
- Just to name a few!
How Images Are Obtained
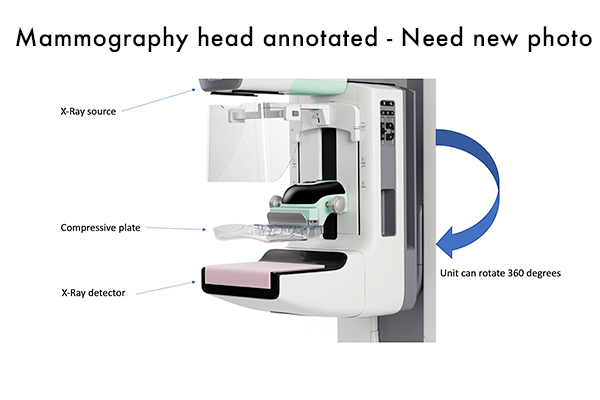
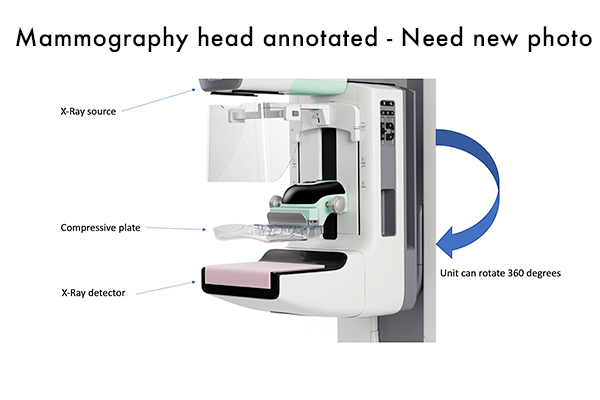
- Breast is compressed between a plastic compression plate and the X-ray detector.
- Why compression is used:
- Compression helps spread out the fibroglandular tissue making it easier for radiologists to detect abnormalities.
- Limits motion artifact which also helps aid in detection.
- More compression means less radiation exposure required to produce optimal images.
- Unit can rotate 360 degrees to obtain different views.
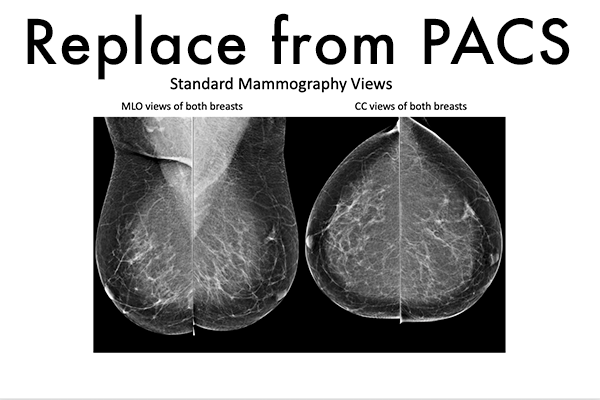
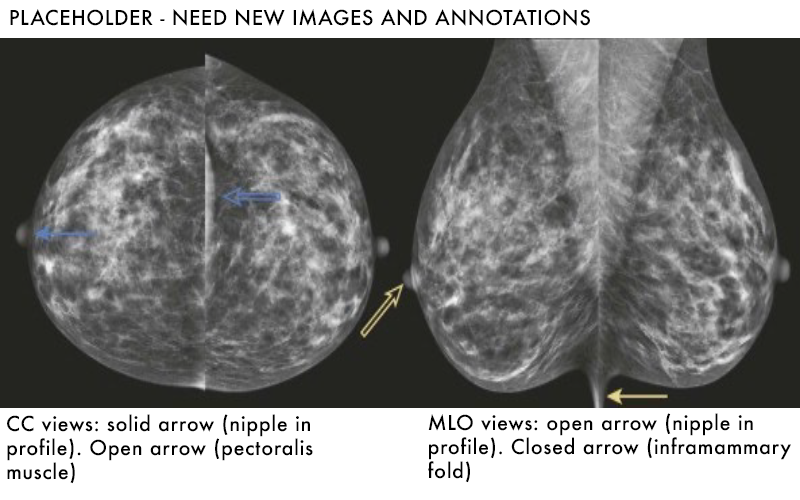
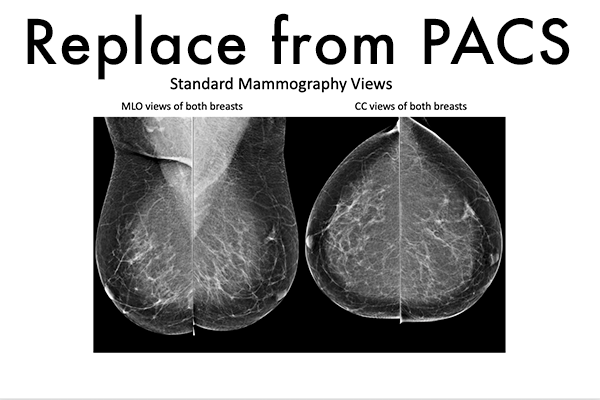
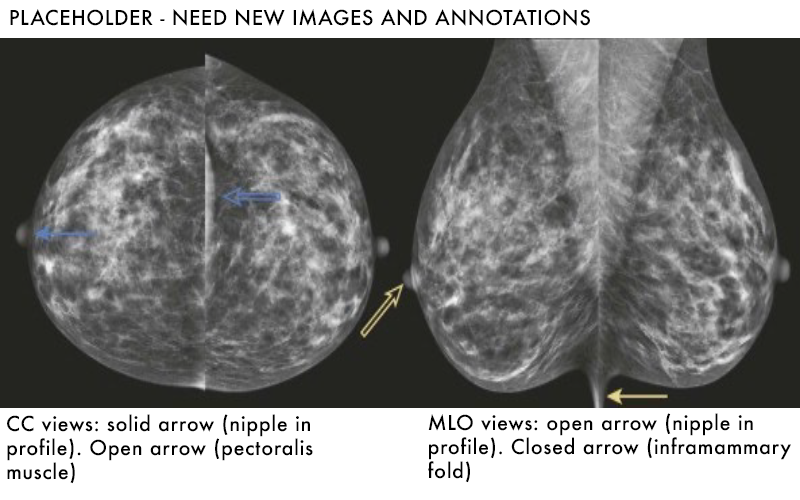
- Cranial-Caudal (CC) and Mediolateral Oblique (MLO) are the standard views obtained on a routine screening mammogram.
Standard Mammography Views
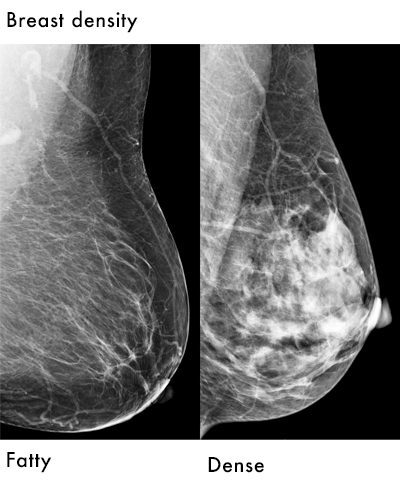
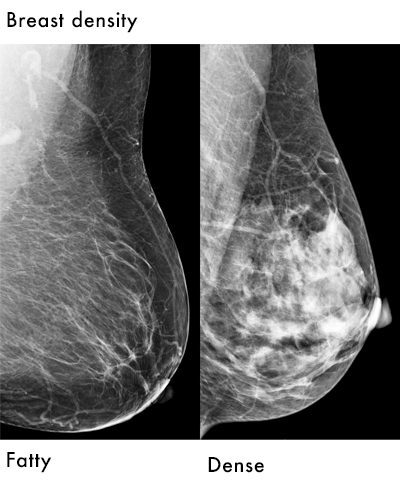
Effects of Breast Density on Mammography
- Varying differences in breast density are seen, which can play a big role in the ability to detect lesions.
- Four main categories of breast densities are assigned to each case.
- Almost entirely fatty
- Scattered density
- Heterogeneously dense
- Extremely dense
Test your knowledge
Placeholder quiz - we may want to craft a different / better question.
Basics of Interpreting Mammograms
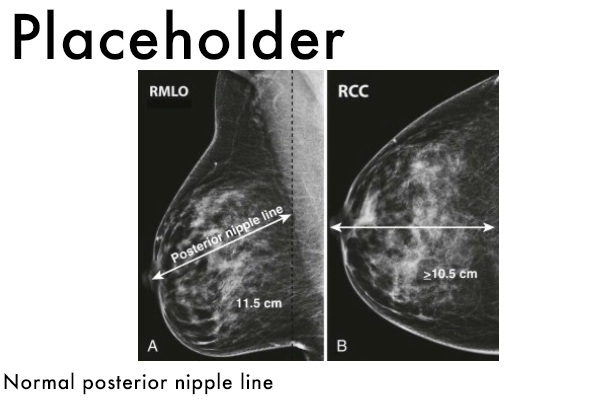
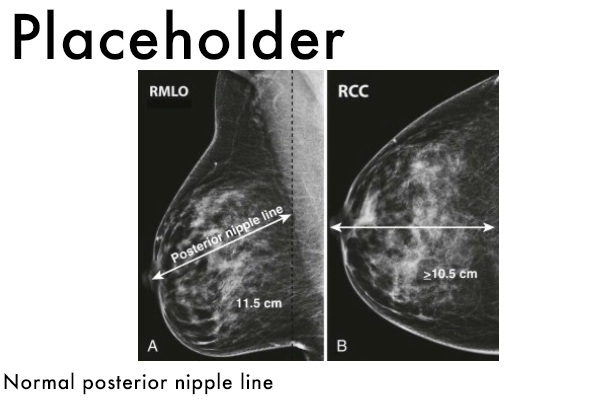
- First step is to determine if the study is technically adequate.
- Nipple should be in profile in at least one view.
- Image should be free of motion or artifact.
- Adequate breast tissue should be included.
- Posterior nipple line: line drawn from posterior nipple on MLO view should intersect with the pectoralis muscle. Line is also measure on CC view, measurements should be within 1.0cm of each other.
- Inclusion of the inframammary fold on the MLO view.
- Inclusion of retroglandular fat
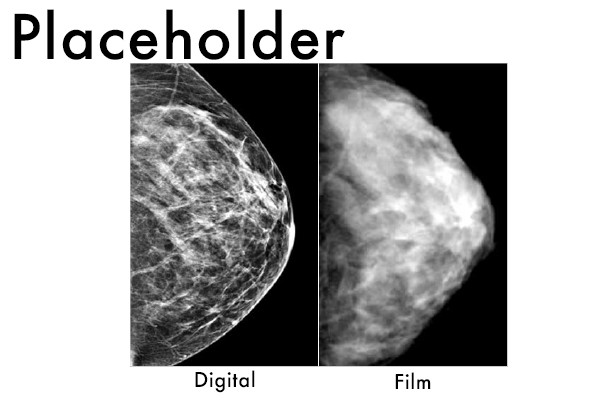
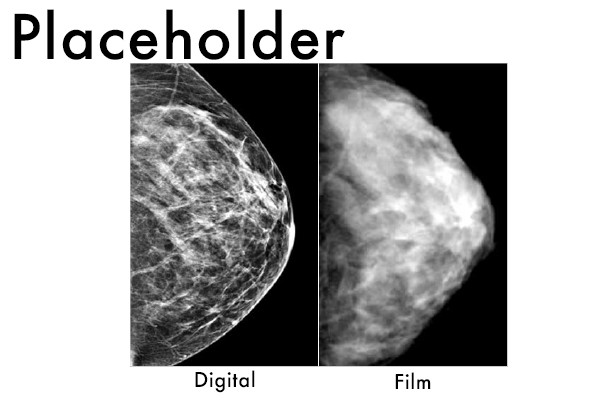
Digital Mammography
- Film was used up until 2000, until FDA approved use of digital mammography.
- No longer use actual film as the detector, rather a digital detector converts photons into a digital signal.
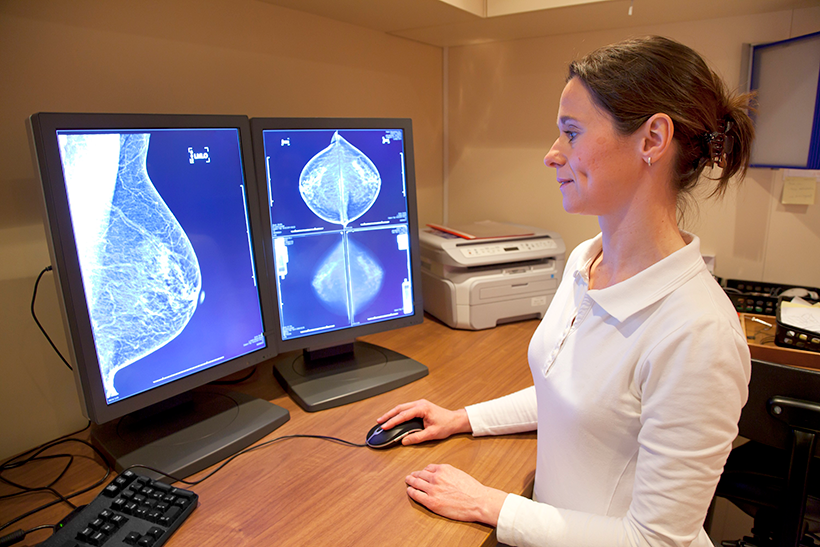
- Digital signal can be viewed on high resolution monitors instead of older light boxes.
- Digital mammography has nearly completely replaced film at this point.
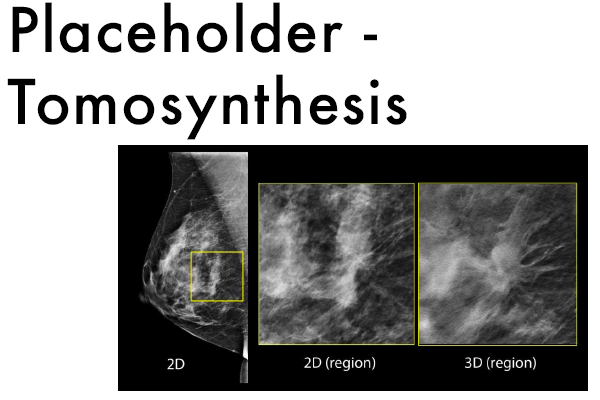
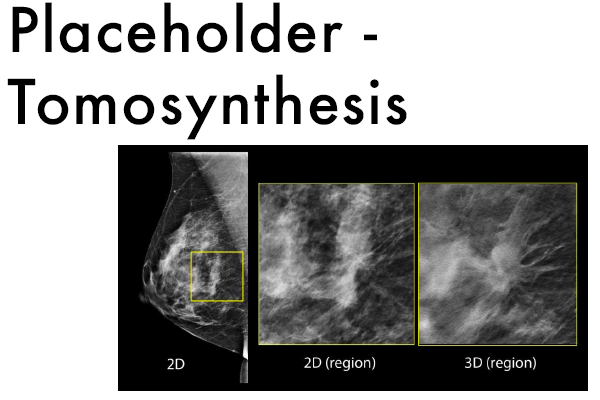
- Digital mammography also allows use of tomosynthesis (3-D mammography).
- Thought to help aid in detection of subtle lesions.
Tomosynthesis