At UVM’s College of Arts and Sciences, you'll have extraordinary access to distinguished scholars and scientists, in and out of the classroom; 40 percent of our students engage in faculty-mentored research.
You'll also gain experience through engaging internships, service learning, or study abroad experiences, taking advantage of UVM partnerships throughout Vermont, the U.S., and abroad. While building knowledge and skills in your area of study, you’ll learn how to analyze data, identify connections, and communicate complex ideas – abilities employers want and society needs.
academics
What makes us special

Explore humankind
Humanities study at UVM focuses on human beliefs, expression, and philosophy throughout history and around the globe, particularly within our School of World Languages and Cultures. Classrooms near and far provide the ultimate experience through exhibits, performances, field trips, and more.

Immerse yourself in the arts
A UVM fine arts journey centers on creative inquiry and instruction. Our School of the Arts programs offer a rich, student-centered environment of technical advancement, exploration, professional development, and experiential learning for a lifetime of arts engagement.

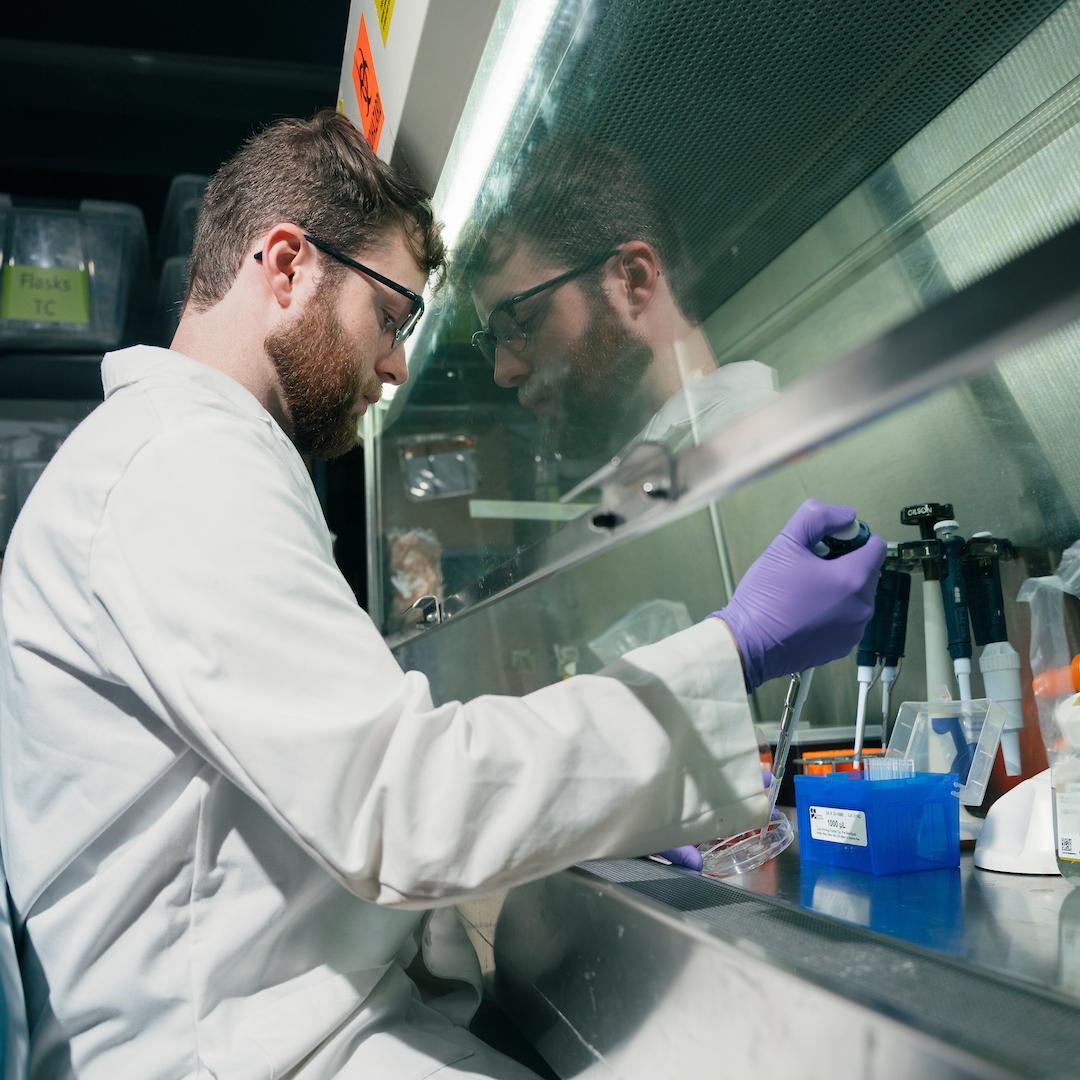
From natural to social science
Accessibility to our college’s faculty and their world-changing research is a game-changer as you examine the physical world and its phenomena, or human behavior and the human condition through the lens of economics, politics, geographics, race, and gender.
By the numbers
- 94% of 2019-2021 graduates were employed or continuing their education within 6 months of graduating
- 40+ majors offered in the college
- 92% of CAS students have at least one internship or other intensive field training experience